By 2050 estimates suggest that deaths caused by common infection could outnumber those caused by cancer, and it’s well known that seniors are among those at greatest risk. Infection is the most common cause of transfer to hospital and readmission, and the fact is, hospitals themselves are breeding grounds for further infection, creating more risk for those admitted.
The cycle can be a vicious one.
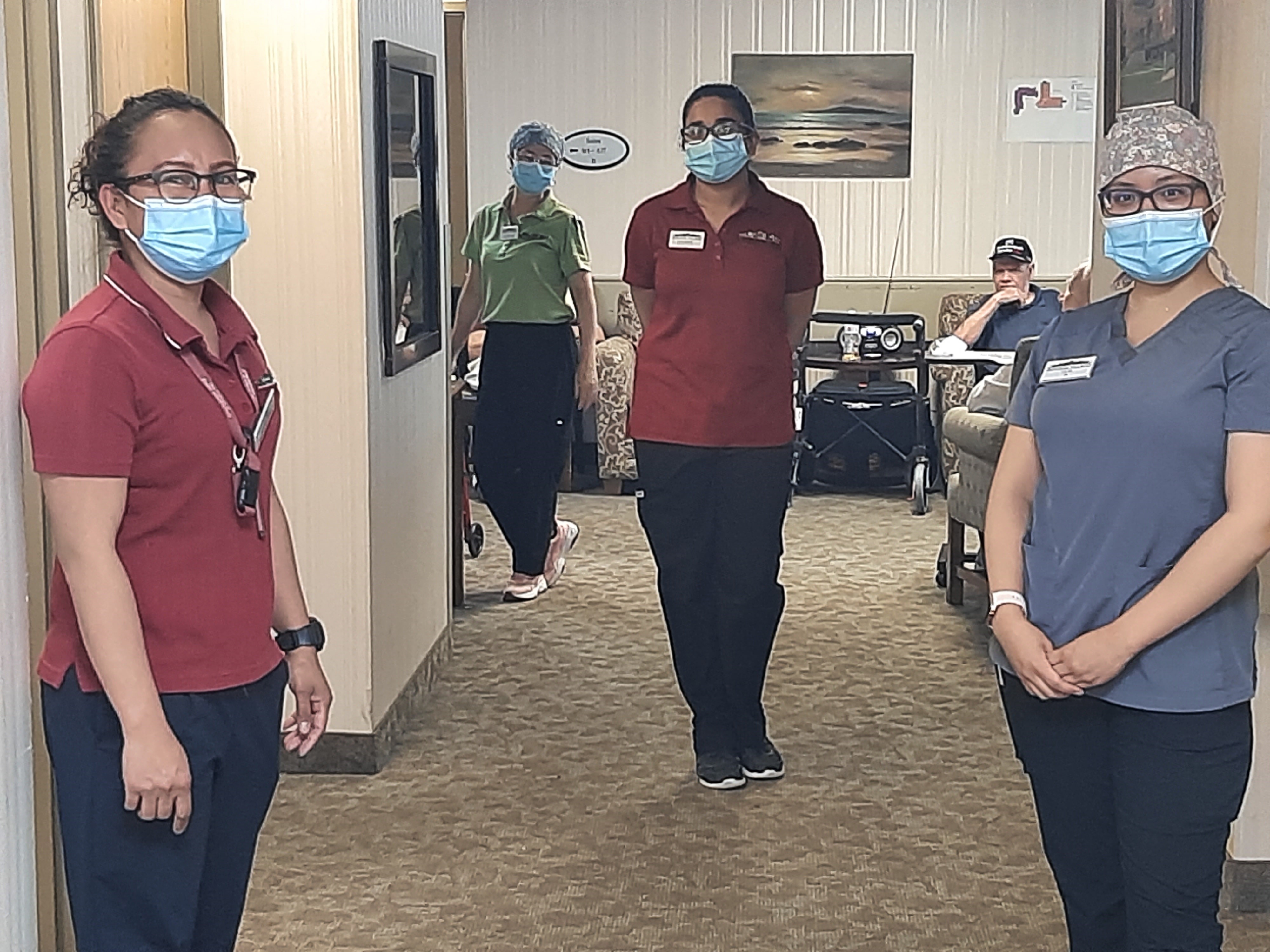
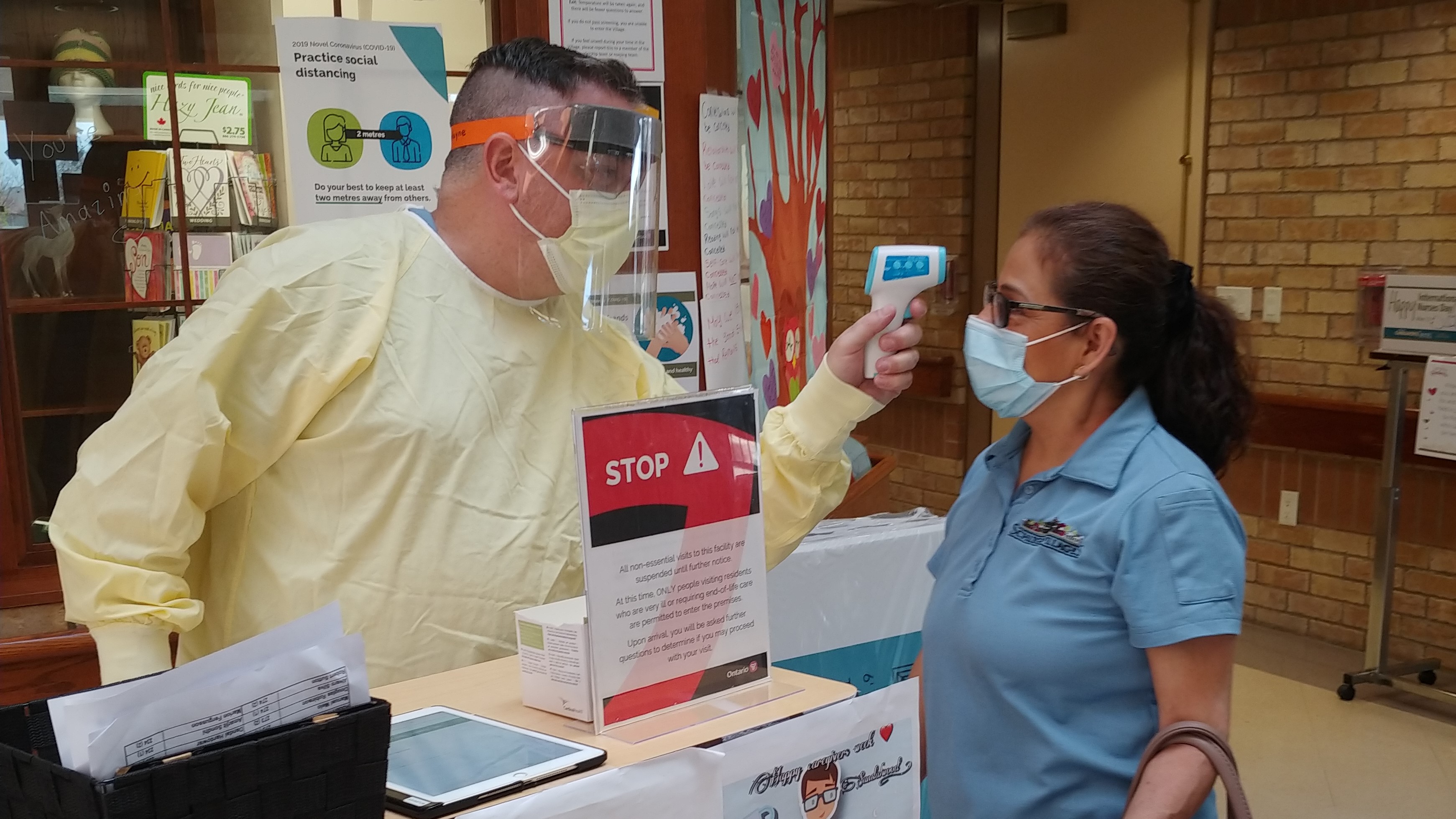
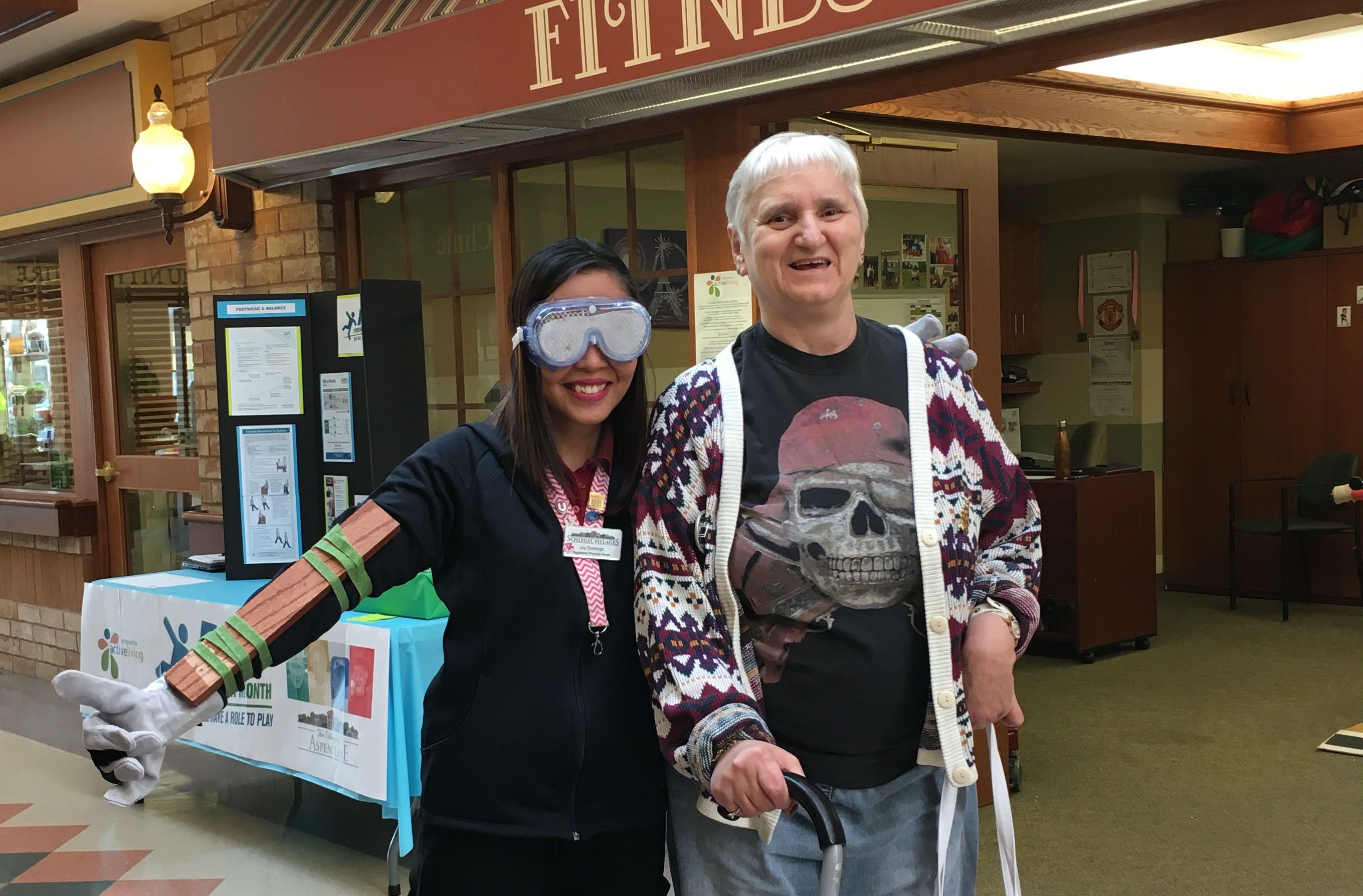
For an organization like Schlegel Villages, these basic facts make infection control a top priority and it’s why for the past two years, a small team within the Support Office has been working diligently towards the creation of an enhanced surveillance tool to help identify outbreaks earlier, collect and collate data, identify trends and ultimately decrease infections.
With support from Public Health Ontario, Jessica Jasper and Wendy Miller have developed a new tracking system to help eliminate the guesswork behind infection identification. It also allows teams to assess trends, helping them zero in on reasons why certain villages or neighbourhoods are seeing increased frequency of certain infections.
Consider one of the more common infections: when a resident in a long-term care home seems abnormally tired or has a fever, for example, it’s often automatically assumed they have a urinary tract infection and they are treated as such with antibiotics, despite the fact there is no confirmation of an actual infection.
This is a dangerous trend.
“More and more organisms are becoming resistant to antibiotics because we continue to treat without meeting the case definitions for infections,” Wendy says. “We’ve had cases where a resident goes hospital with a fracture or weakness and will come home on antibiotics with a diagnosis of an infection. We’ve even had cases where the lab has identified no infection and still the resident comes back with an antibiotic.
“We need to stop this practise or we are going to get the point where we will not be able to treat basic, real infections.”
The new surveillance system Jessica and Wendy developed can help monitor symptoms, providing a much more accurate reading of what a resident is feeling day-to-day.
“I can hand my nurses a tool and have them take it to the doctors and ask, ‘why are we treating 27 residents without an actual confirmation that it is a urinary tract infection?’ ” Jessica says.
There are other options to take care of it naturally, she points out, so with the standardized surveillance information, teams will be armed with the necessary knowledge to make informed decisions.
“In order to have that conversation, though, they need the data,” Jessica says.
The new system has been in operation for less than a year and there are still adjustments to be made as feedback and results come in from across the Villages, but early results have been positive. There has been a decrease in misdiagnosed infections and heightened collaboration, but more needs to be done to scale the system up.
Enhanced infection control will always remain a top priority, however, for increased risk of infection not only affects residents but also team members and families. “We need to do everything we can to keep them safe, happy and infection-free,” Wendy says.
- Previous
- View All News
- Next