Schlegel Villages embarks on a redesign of supports for those living with dementia
By Kristian Partington
When Mary-Beth Wighton was diagnosed with frontotemporal dementia at the age of 45, she distinctly remembers the shock that followed as the doctor told her: “Go home and get your affairs in order.”
Her life, in such a short span of time, had been pulled out from under her. Her driver’s license was taken on the spot and as she sat in her car after that meeting, she was left to wonder just how long she had to live. There was no other side to dementia that day. In a few sentences the doctor had drawn a picture in her mind of the worst-case scenario, which typically presents in the latest stages of the disease’s progression, and there was no life in between that unknowable future and the moment she was in.
She and her partner Dawn left the hospital that day swirling amidst a cloud of despair, holding nothing more than a pamphlet about Pick’s disease and a number for the local Alzheimer’s Society.
“The whole initial part of it was terrible, “ she says, pointing to the way in which she was presented with the diagnosis. “The way that the words roll out of a doctor’s mouth really does play into your initial response.” Unfortunately, her doctor failed to see that it is possible to live well with dementia. The stereotypes and stigma that hover over the word dementia were perpetuated by this medical professional and Mary Beth had to learn for herself that life does not end at the diagnosis.
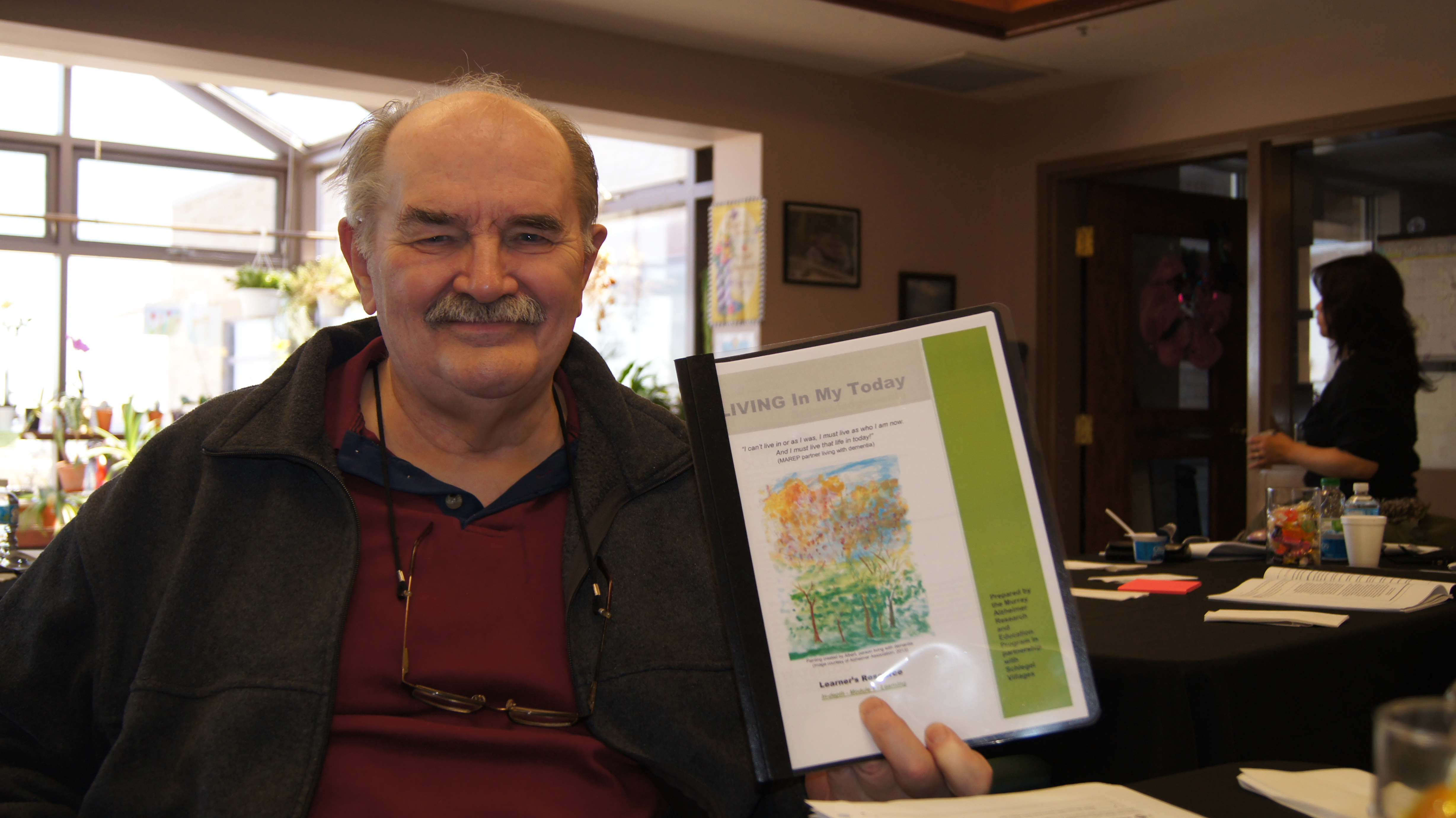
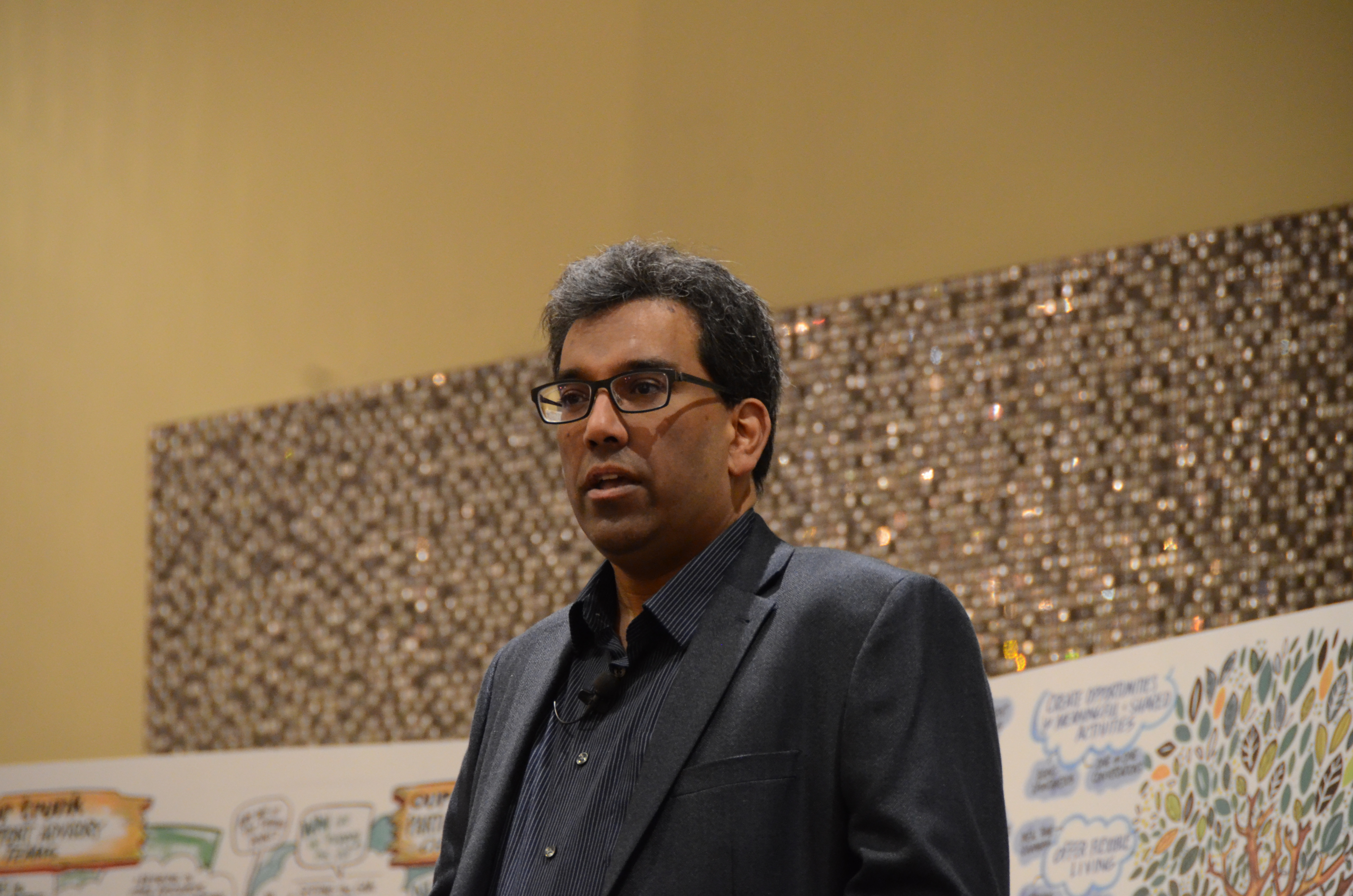
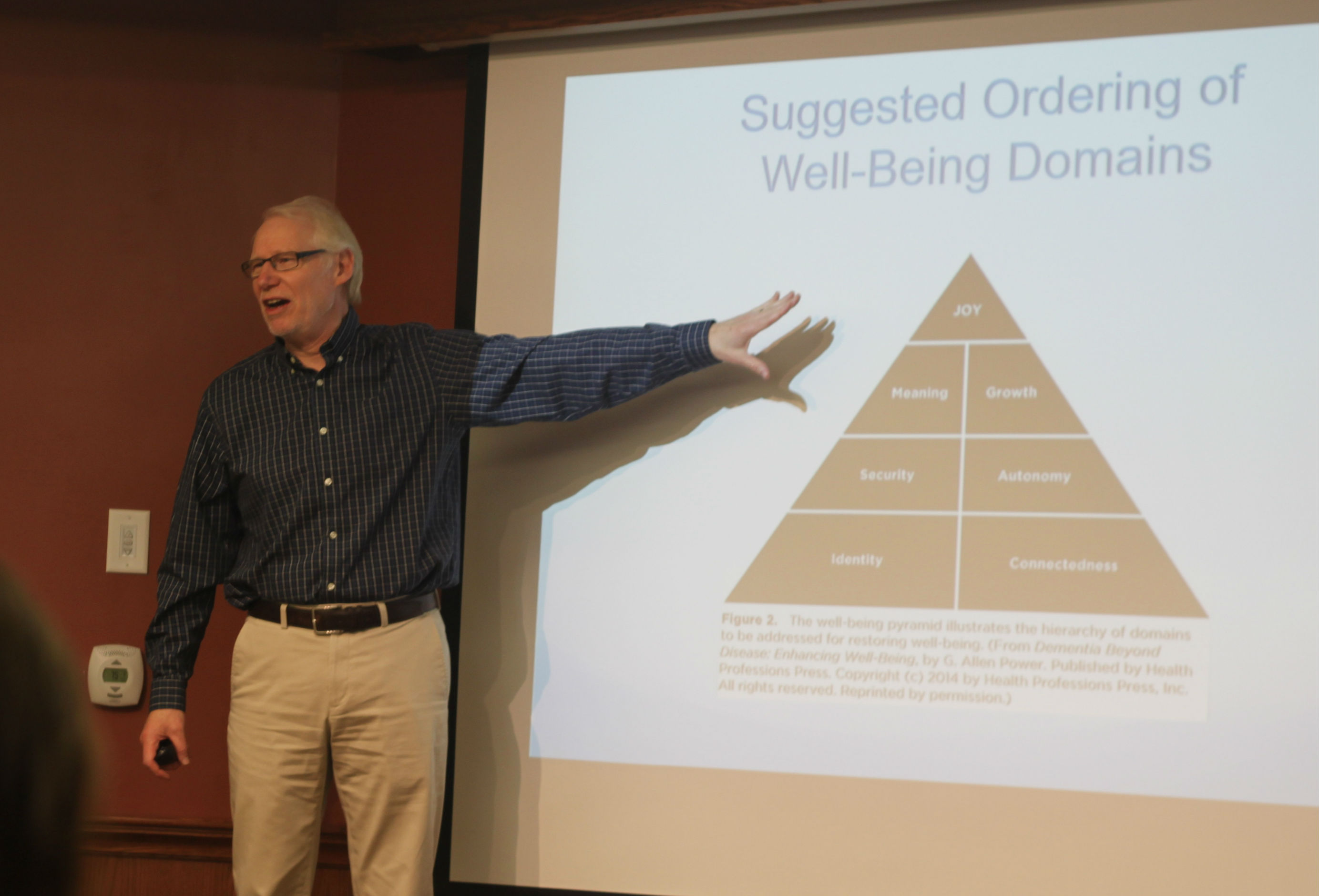
Four years later, she’s as busy as she’s every been, challenging societal views and stigma as an advocate with the Ontario Dementia Advisory Group and she recently joined Schlegel Villages as a member of the Dementia Program Development Advisory Committee, which met for the first time on Feb. 17. This committee, comprised of village and support office team members, residents, family members and outside thought leaders like Mary Beth and dementia specialist Dr. Allen Power, will deeply explore the organization’s entire approach to dementia care and make recommendations to strengthen supports and ensure that every resident, no matter their cognitive ability, is able to live their life to the fullest.
“The better that we hit stigma in the middle of the eye and break it down, then the busier we are getting,” she says of the advocates she works alongside. “It’s as it should be; we should be so busy trying to help people and educate people and work with people to show that you can live well with dementia, you can contribute.”
A major challenge is the fact that when people are presented with a diagnosis, absent of any hope, a sense of helplessness is immediately set in motion, which can be hard to move past. Within Schlegel Villages and beyond, Mary Beth and the committees she’s part of hope to counter these entrenched, misguided notions and offer new perspective.
What sets Schlegel Village’s apart, she says, is the fact that the organization is seeking the input of people who are living with dementia from the beginning of this process. “What happens in many, many projects is they’re already basically half way through the project and have already made key decisions about the outcome and then they bring someone in with dementia, which is like we’re just supposed to nod and say it’s okay. It’s absolute tokenism.”
There’s a sense of reassurance in Mary Beth’s mind to see an organization that sincerely values the experience and opinions of those who live the reality of dementia every day, and she’s eager to see where the committee leads Schlegel Villages.
- Previous
- View All News
- Next