Schlegel RIA Innovators offer solutions for the needs of tomorrow
When Ontario’s Deputy Minister of Health and Long-Term Care addressed nearly 200 people who’d come together for the annual Schlegel Villages/ RIA Innovation Summit in June, he described the hypothetical case of “Eve”. (Click here for previous story.)

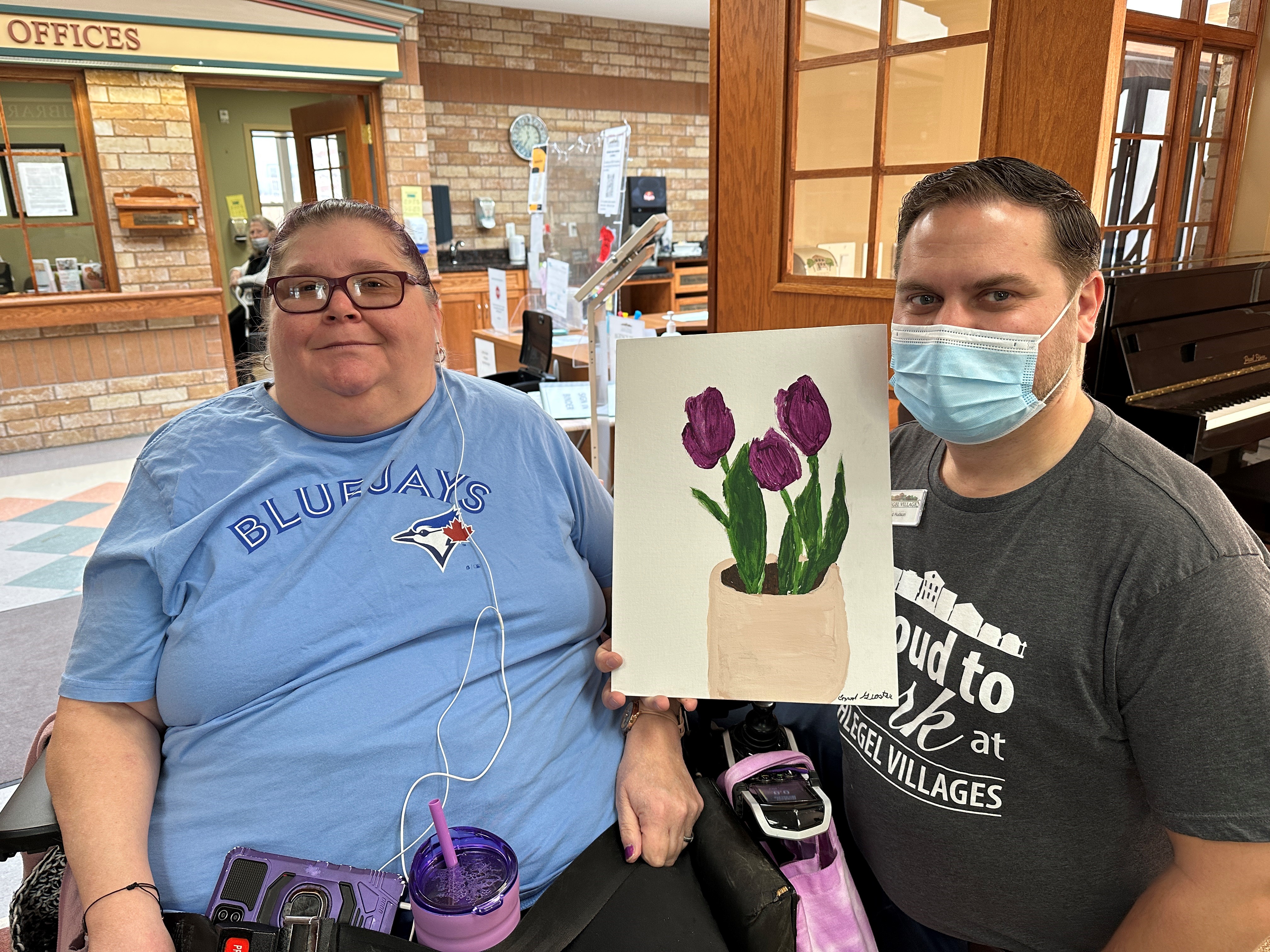
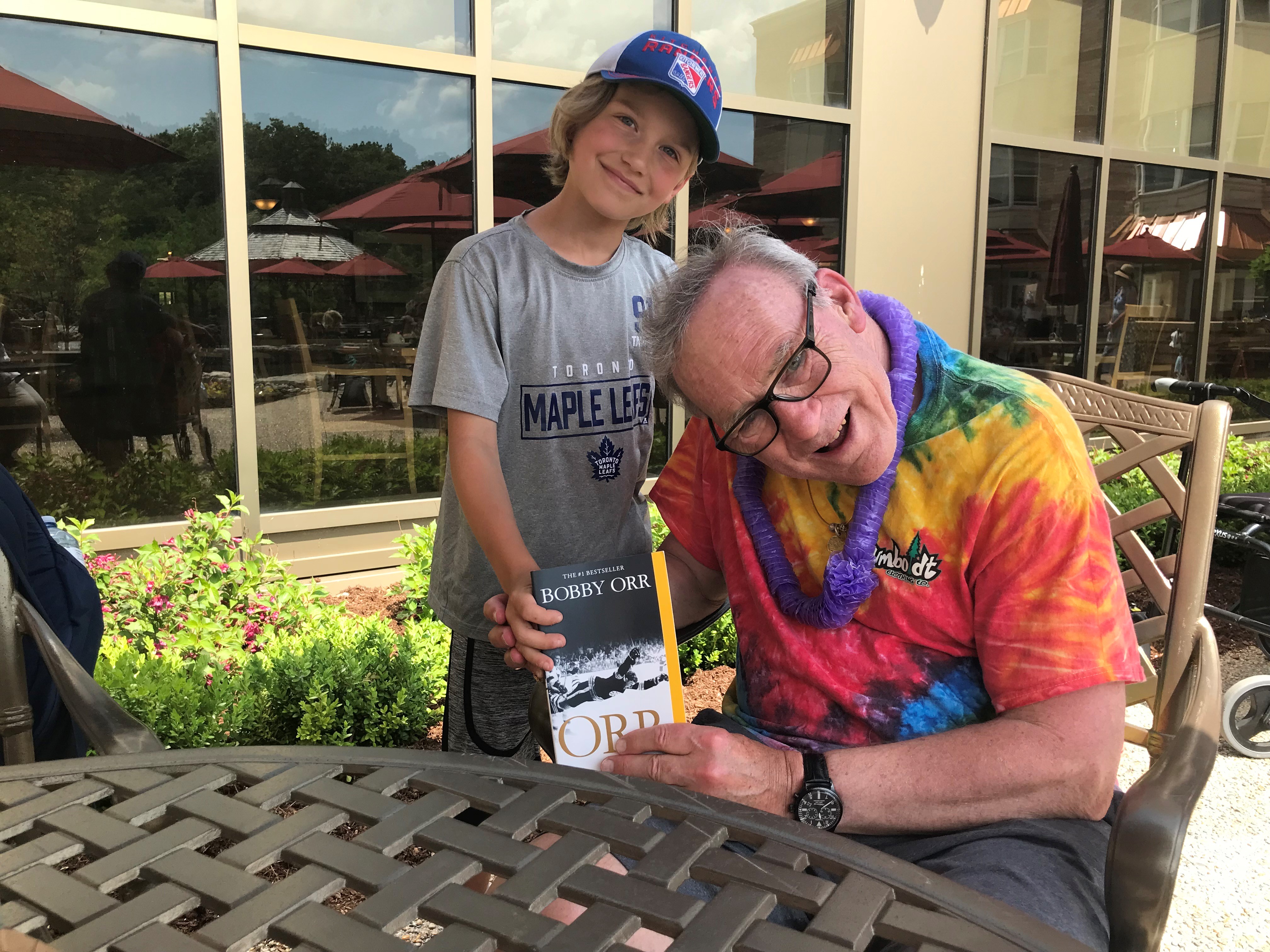
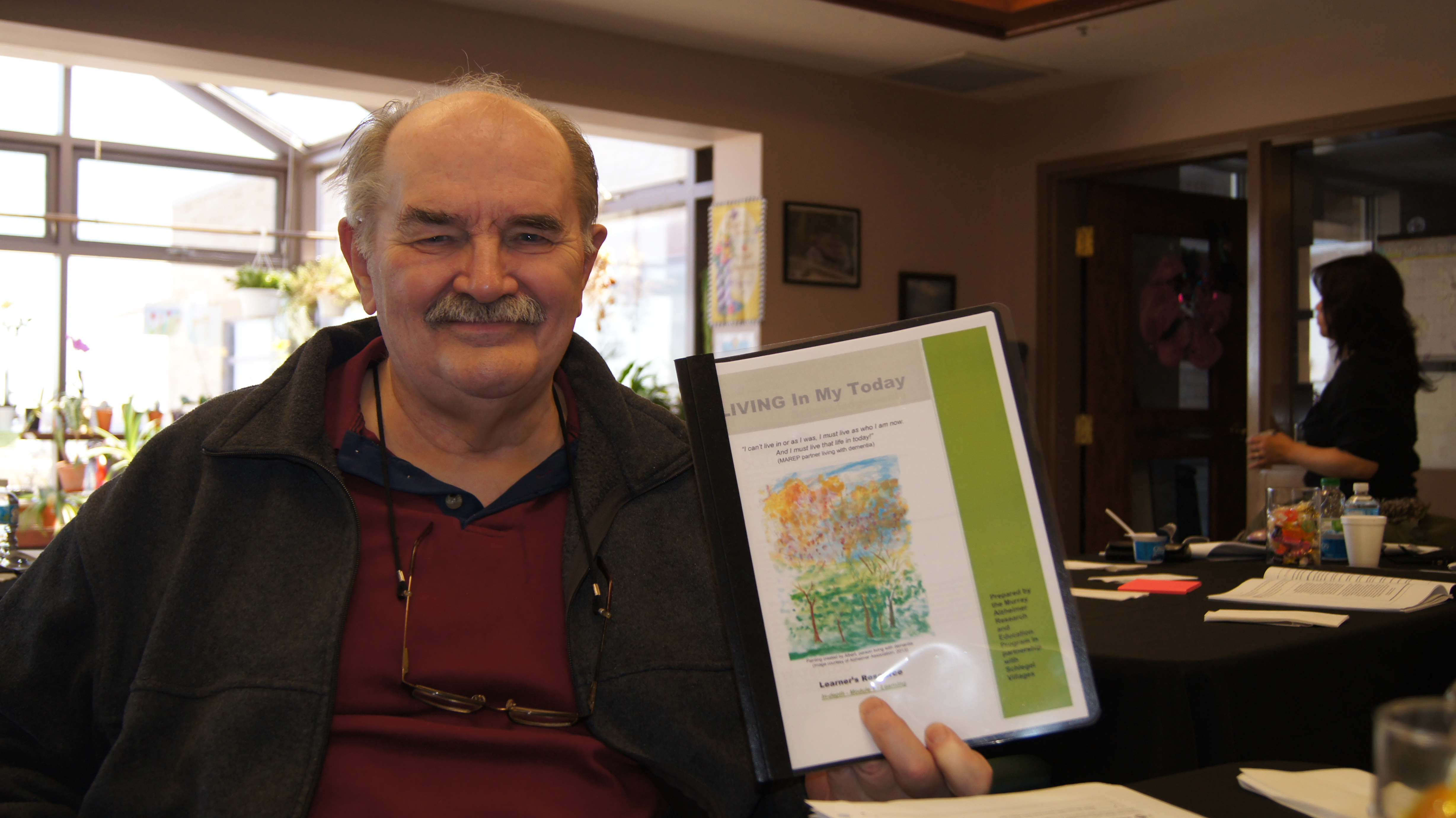
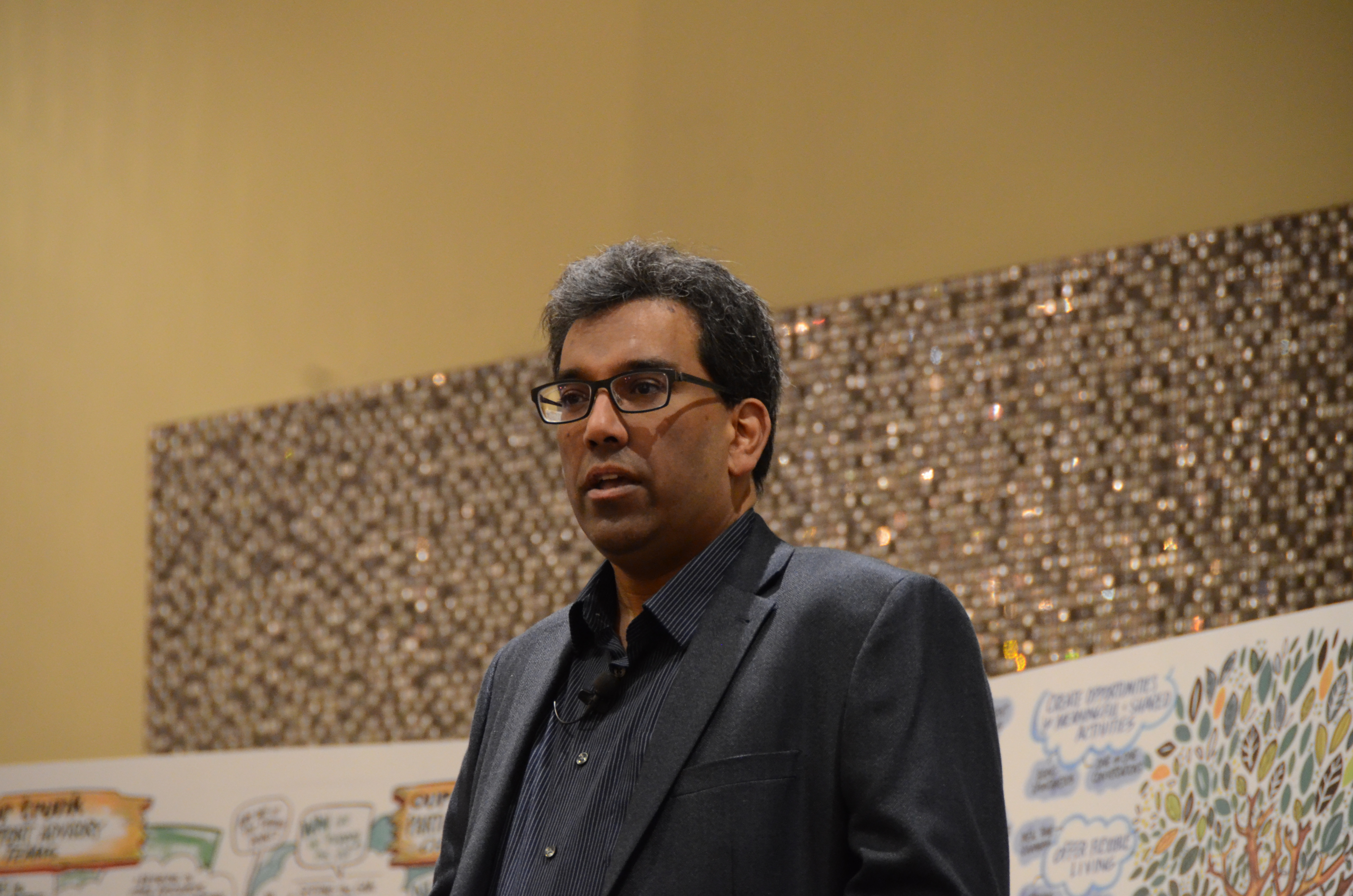
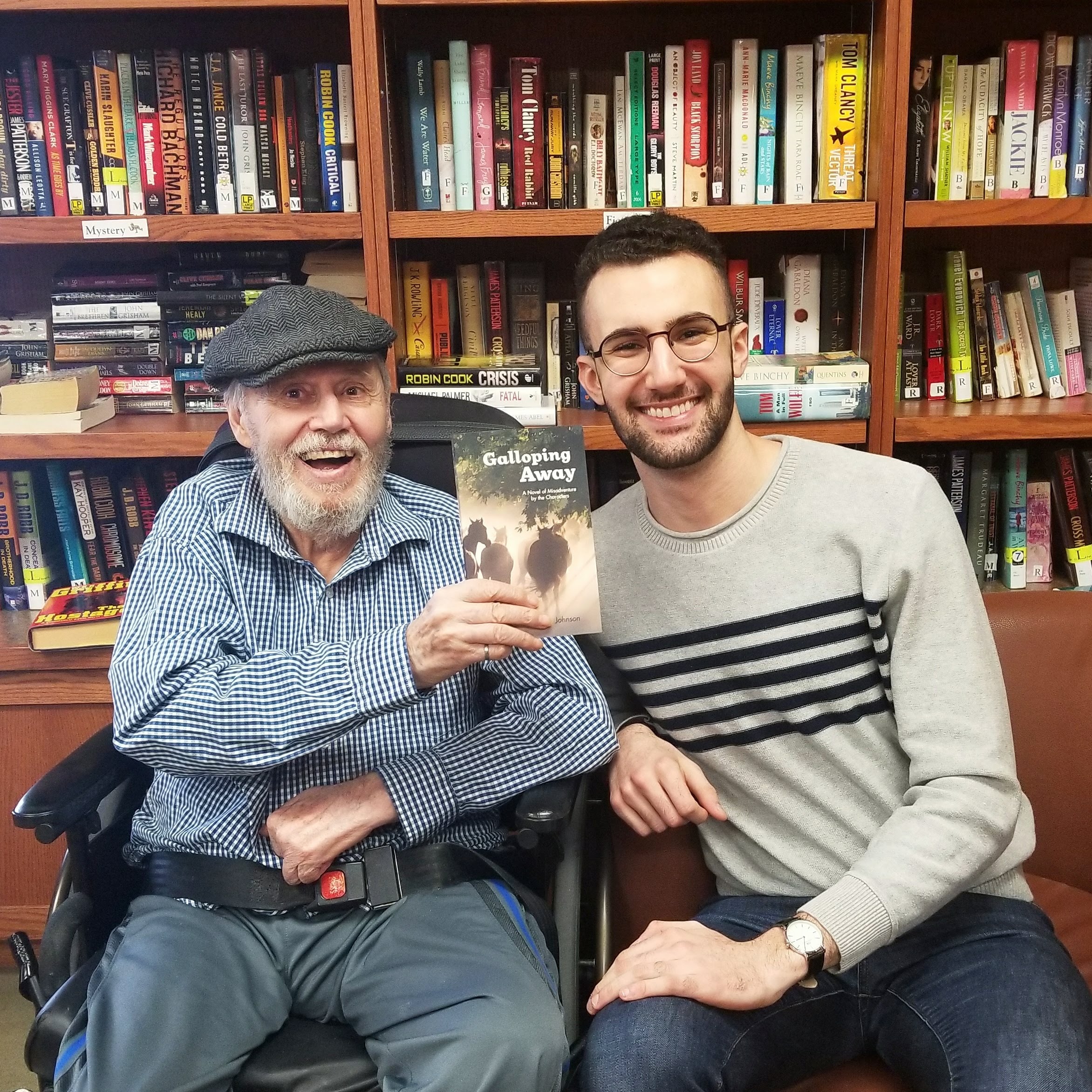
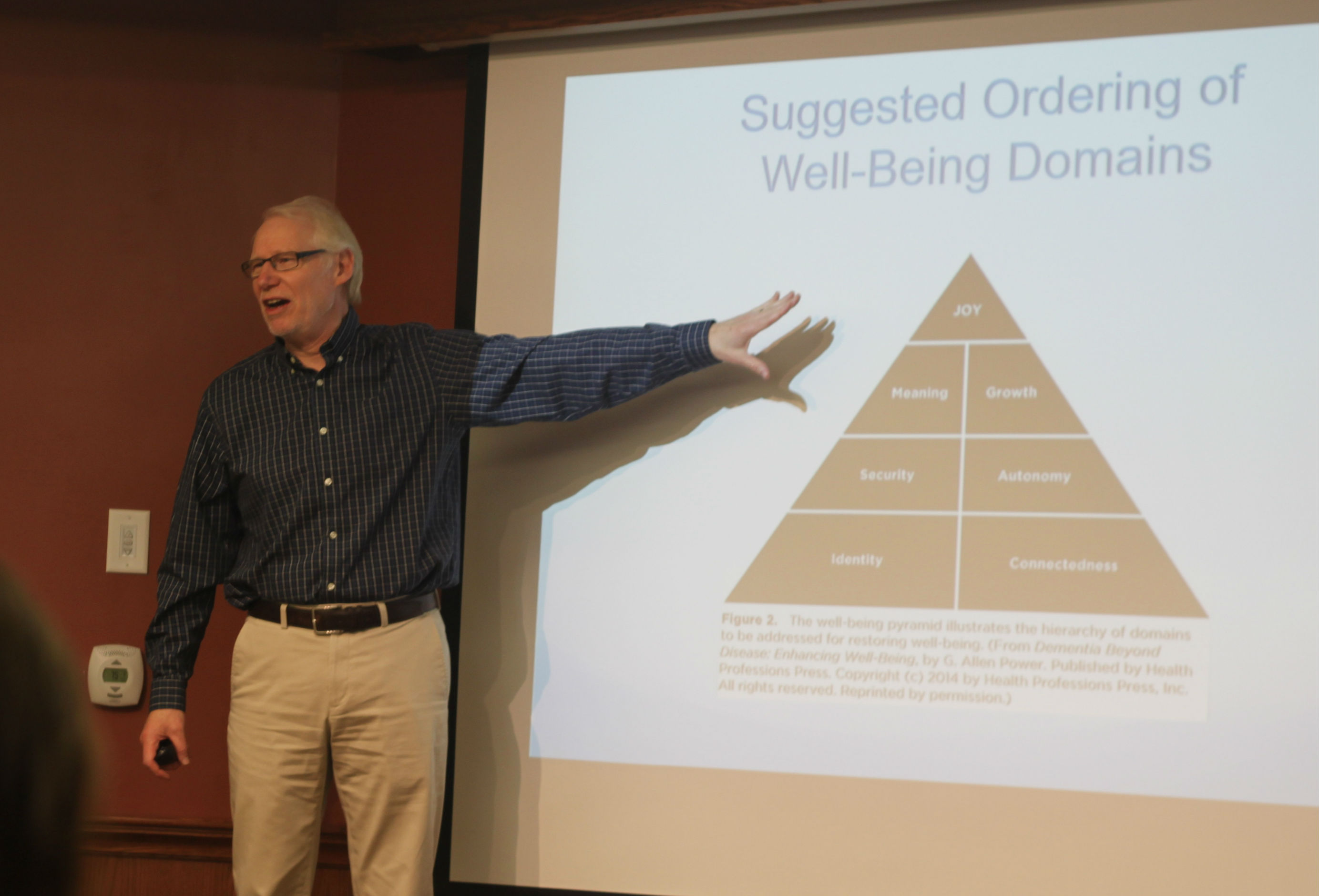
Dr. Robert Bell chats with Schlegel/RIA Innovators following
his keynote address at the 2017 Innovation Summit.
Dr. Robert Bell challenged the audience, comprised of a range of stakeholders from the elder-care sector, to consider the future needs of an aging population, and Eve, who at 86 “fell off an independence cliff” after breaking a hip, represented the ever-growing faction of society that will need the greatest of support as the baby boomers enter their late stages of life.
“What does Eve need?” Dr. Bell asked summit attendees.
Margaret Stinson, a resident from the Village of Arbour Trails, suggested communication is of utmost importance when an older adult faces a health crisis such as Eve’s.
RIA research chair Dr. Allen Power spoke of a consumer-driven model of self-directed care, such as what is offered in Australia, where the person in need is effectively given a package of dollars from the system and they control many of the decisions as to how those dollars are spent.
Several strong ideas emerged, but perhaps most compelling was the description of a pilot project that ran for 10 months at the Village of Taunton Mills in Whitby in 2009-10. At the time, The Central East Local Health Integration Network (LHIN) was looking to improve the flow of inpatients from Lakeridge Health Corporation who didn’t require full-intensity hospital care but were not yet ready to transfer to their ultimate destination – home or long-term care, for example. Through the pilot, Taunton Mills dedicated 20 beds from its retirement neighbourhood as a Transitional Care Unit (TCU). Over 10 months, the village welcomed 98 temporary residents offering them post-rehabilitation convalescence, post-acute convalescence/restorative care or residential care and reactivation.
Hypothetical Eve is just the type of person who was served by the TCU; following her initial acute care, Eve doesn’t need full hospital treatment - in fact, the hospital can be the most dangerous place for her. Instead she needs a home where she can be comfortable as she regains her strength, a place with access to rehab services and a social life that will help her mind and spirit heal just as her body does.
Of the 98 people filtered through the TCU beds during the pilot, nearly half returned home, a quarter moved into retirement homes (including Taunton Mills where they had become completely comfortable) and 12 per cent moved into long-term care. Beyond the fact that three-quarters of the pilot patients were able to regain their independence, the system itself saved more than $1.5 million during that 10-month period, simply because a hospital bed is the most expensive place a person can receive care.
The experience gained through the continuum of care Schlegel Villages offers and the community connections the organization has groomed over time place it in a prime position to reimagine solutions for the Eves of today and tomorrow. This is why Dr. Bell came to the summit, not so much to teach but to learn. Future health care demand will only be met through innovation, and “the Schlegels are leaders,” he said, following his keynote address.
“Part of the reason they’re able to achieve the economics they have is because they are investing in developing better care. It’s something we absolutely respect and listen to.”
The TCU experience at Taunton Mills and the entire continuum model the organization is working to enhance is a definite part of the solution the system requires. Innovation is the continual quest to improve and enhance this system, and Dr. Bell said the model he sees in Schlegel Villages is a reason the find hope for the future.
- Previous
- View All News
- Next