One of Ontario’s leading health officials poses deep questions to Schlegel innovators
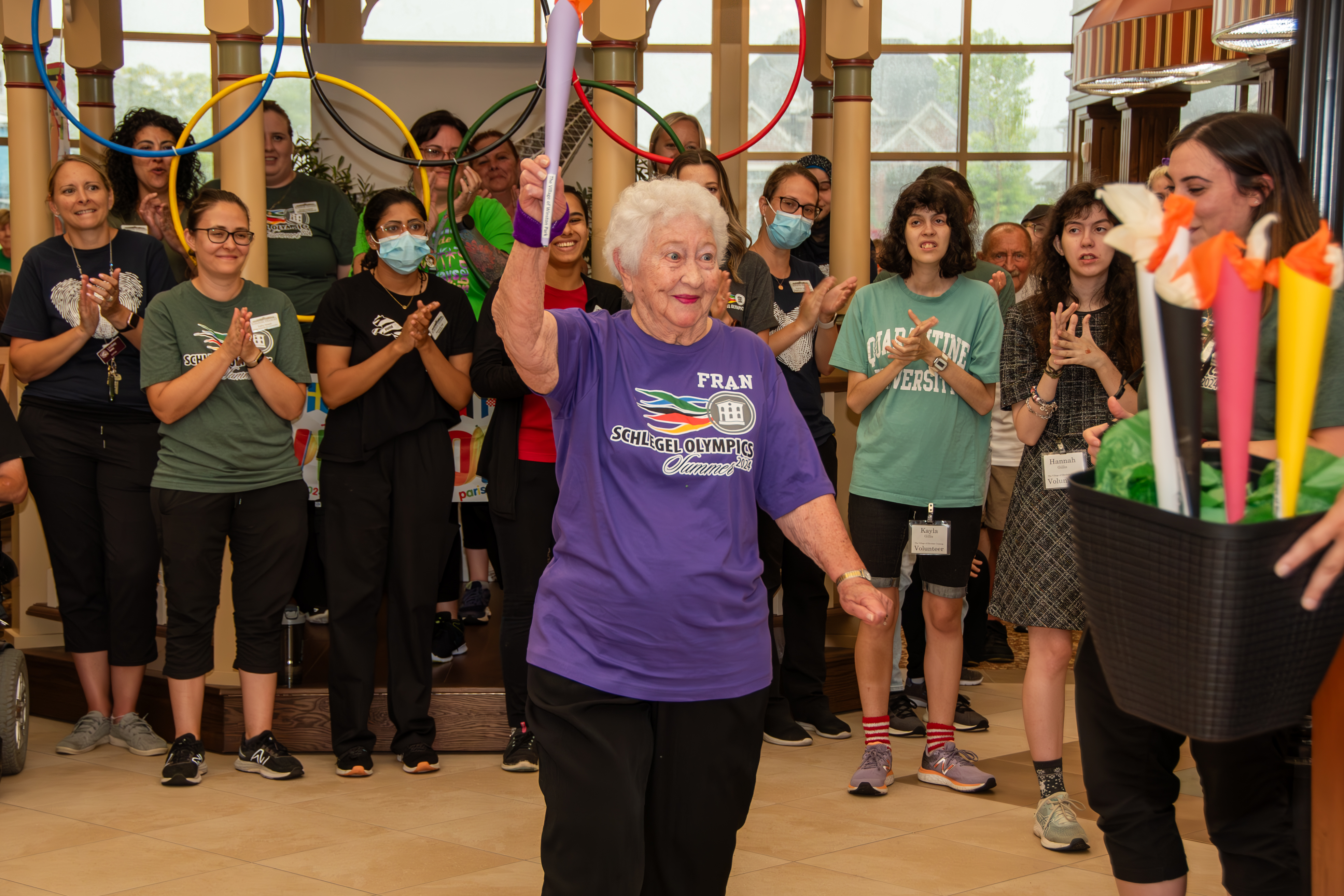
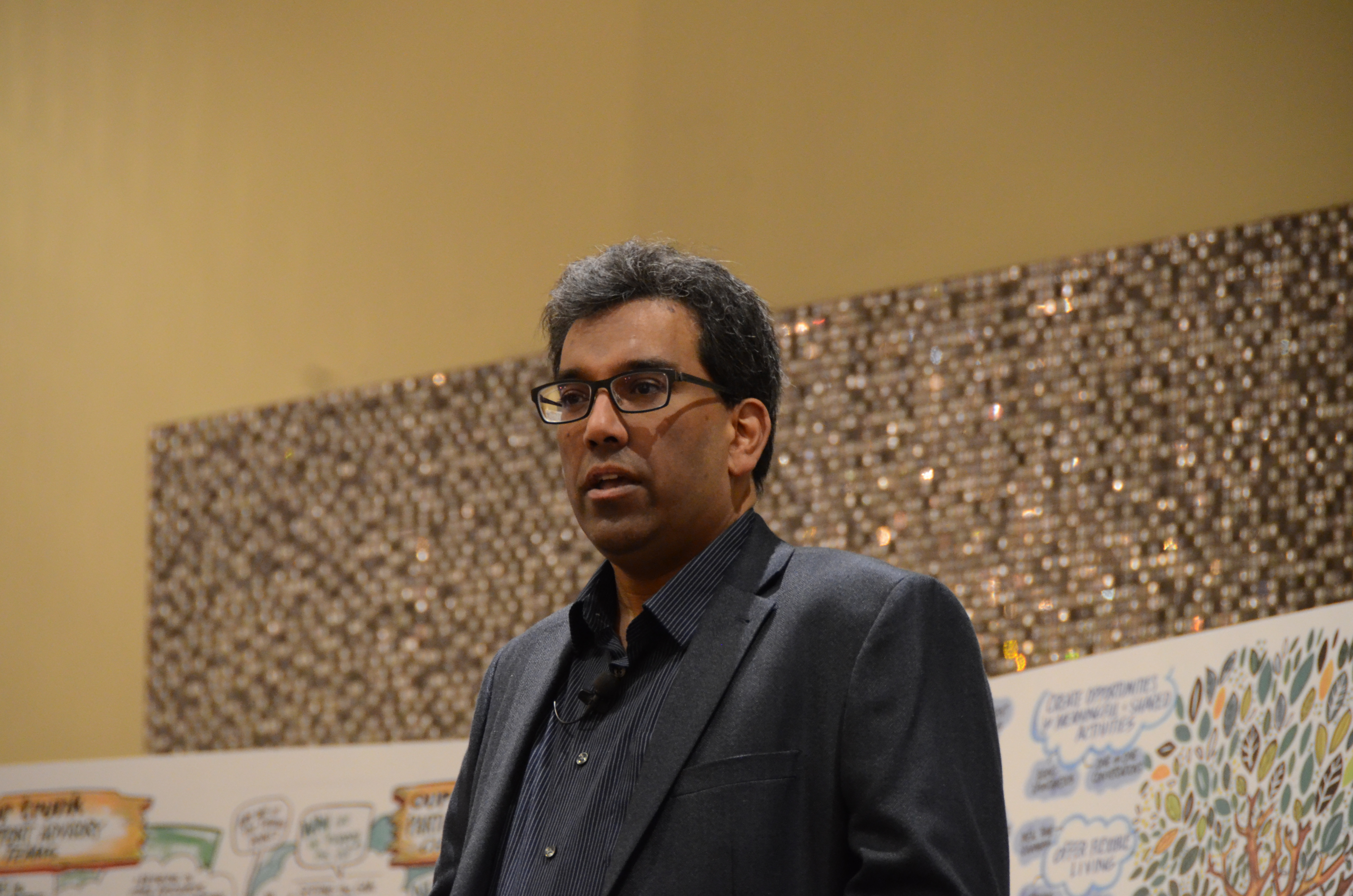
In mid-June, Dr. Robert Bell, Ontario’s Deputy Minister of Health and Long-Term Care, offered a keynote address to open the 3rd annual Schlegel Villages/RIA Innovation Summit.

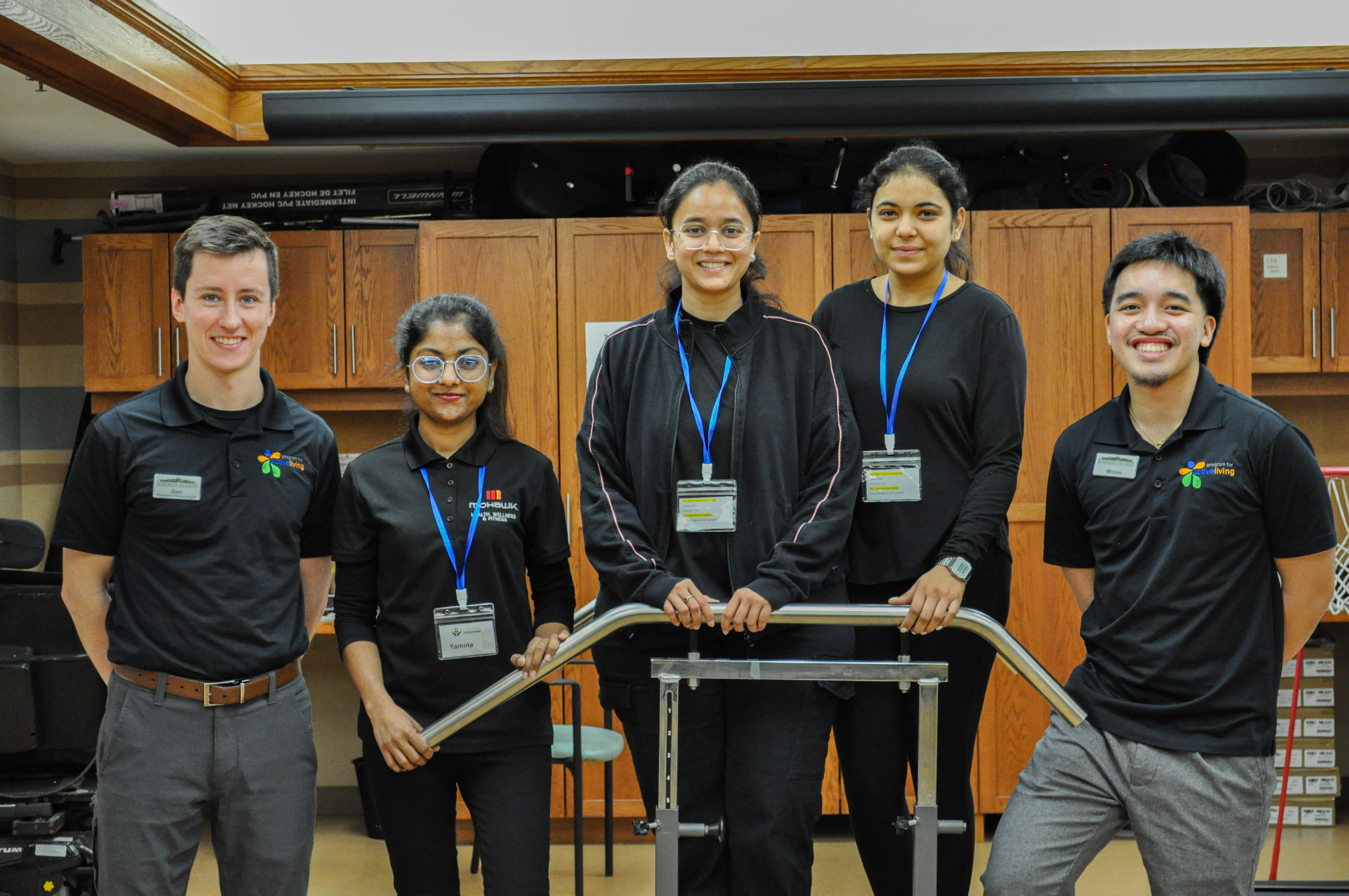
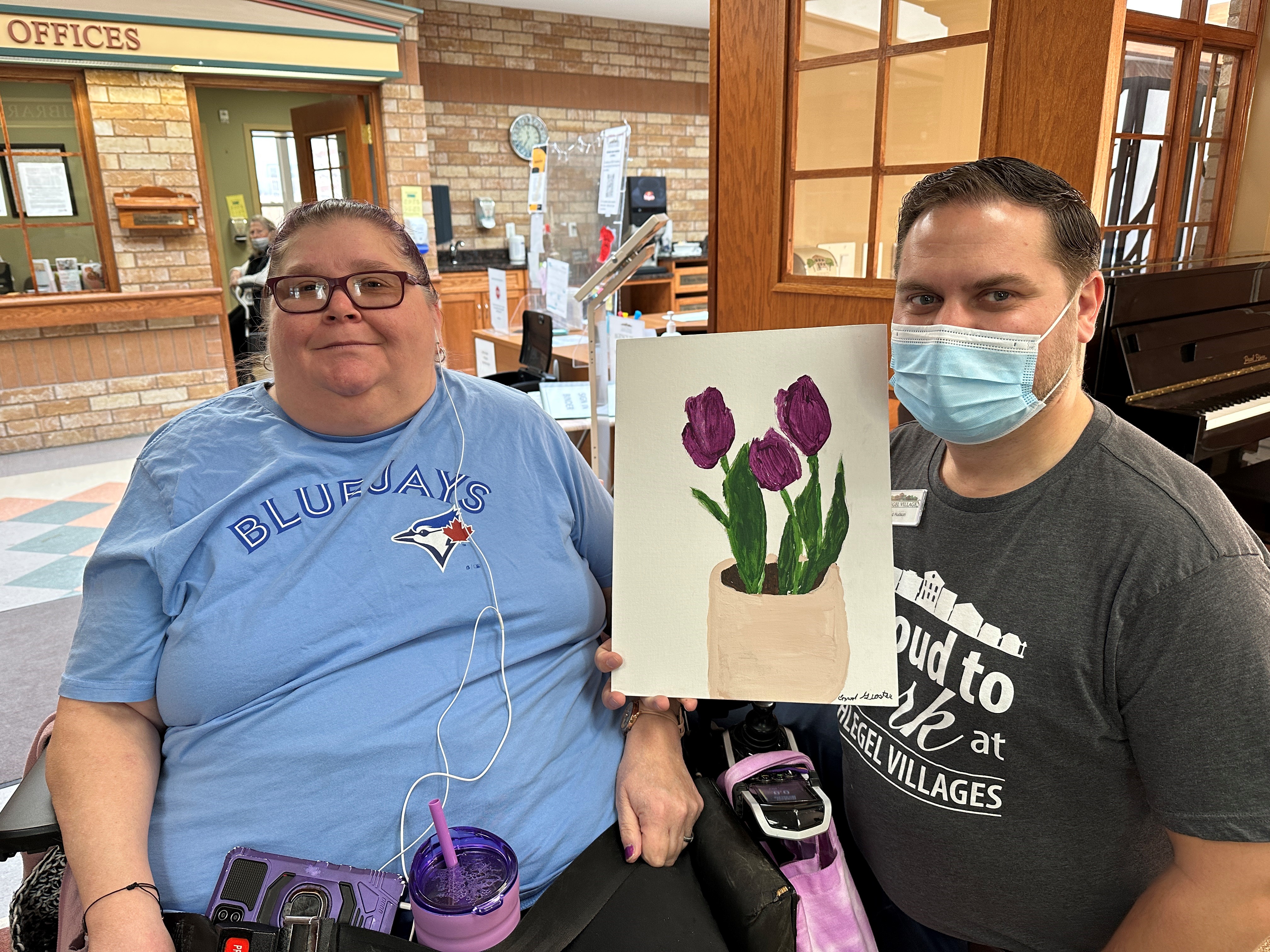
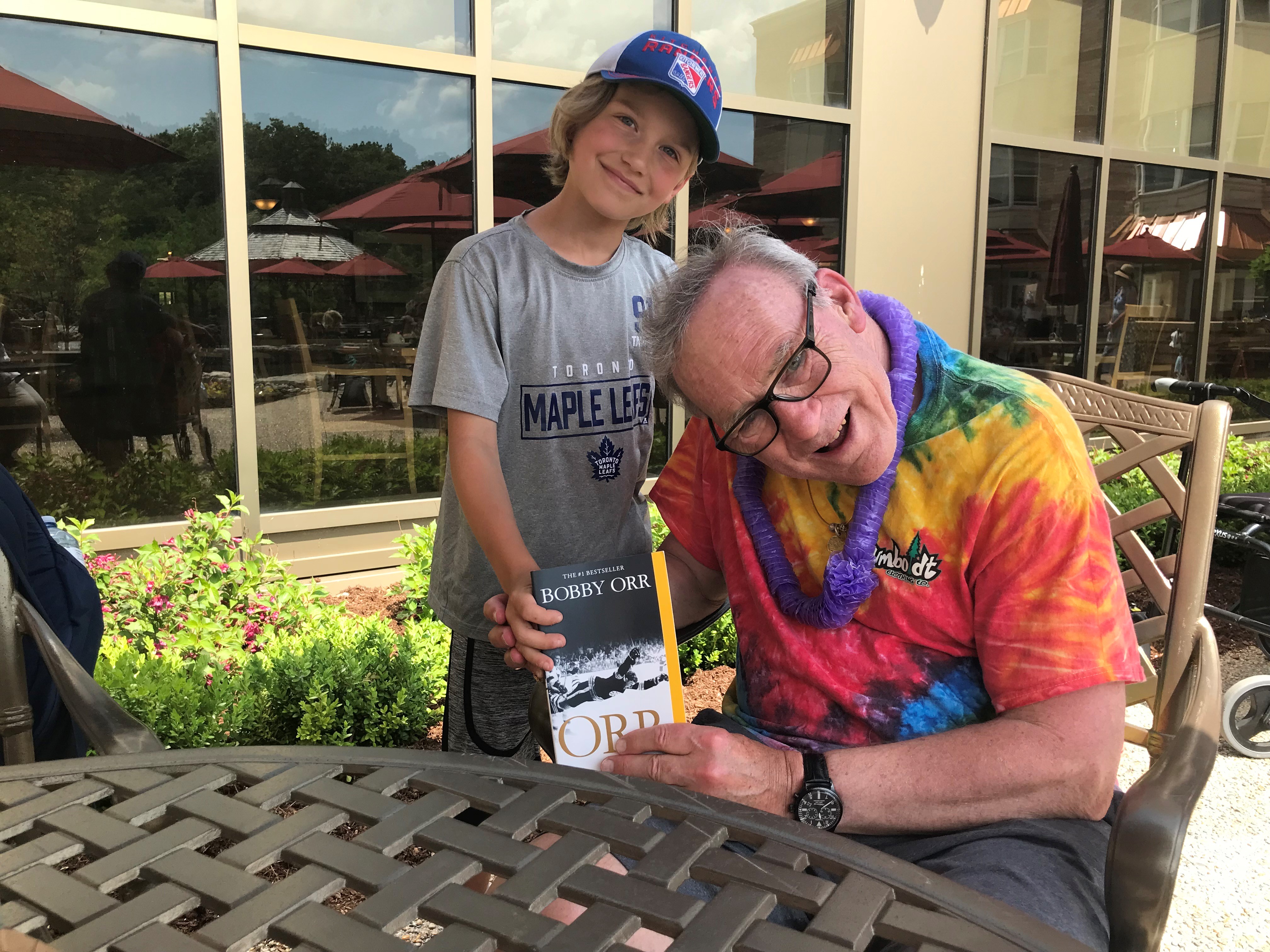
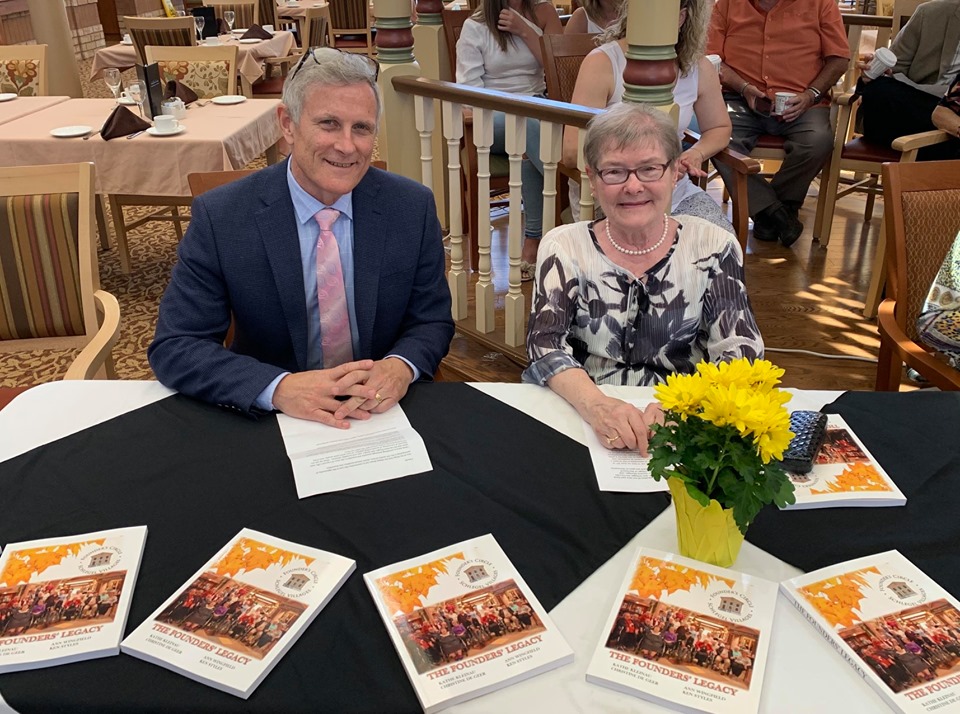
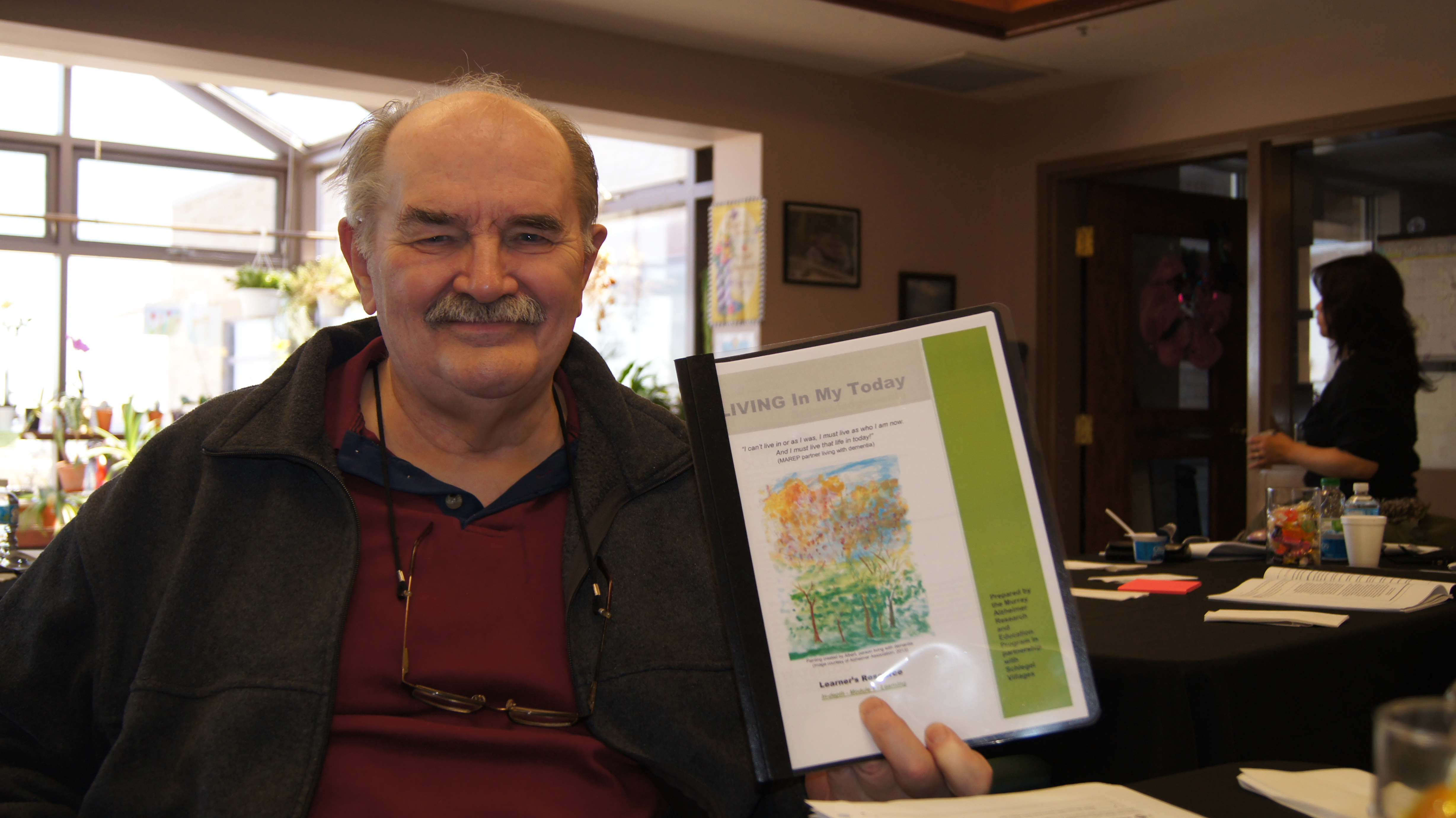
Dr. Robert Bell takes a response from Dr. Al Power during
a keynote address at the Schlegel/RIA Innovation Summit.
He began by describing the very real challenges facing the health care system today, which are destined to compound with the influx of baby-boomers entering their late stages of life.
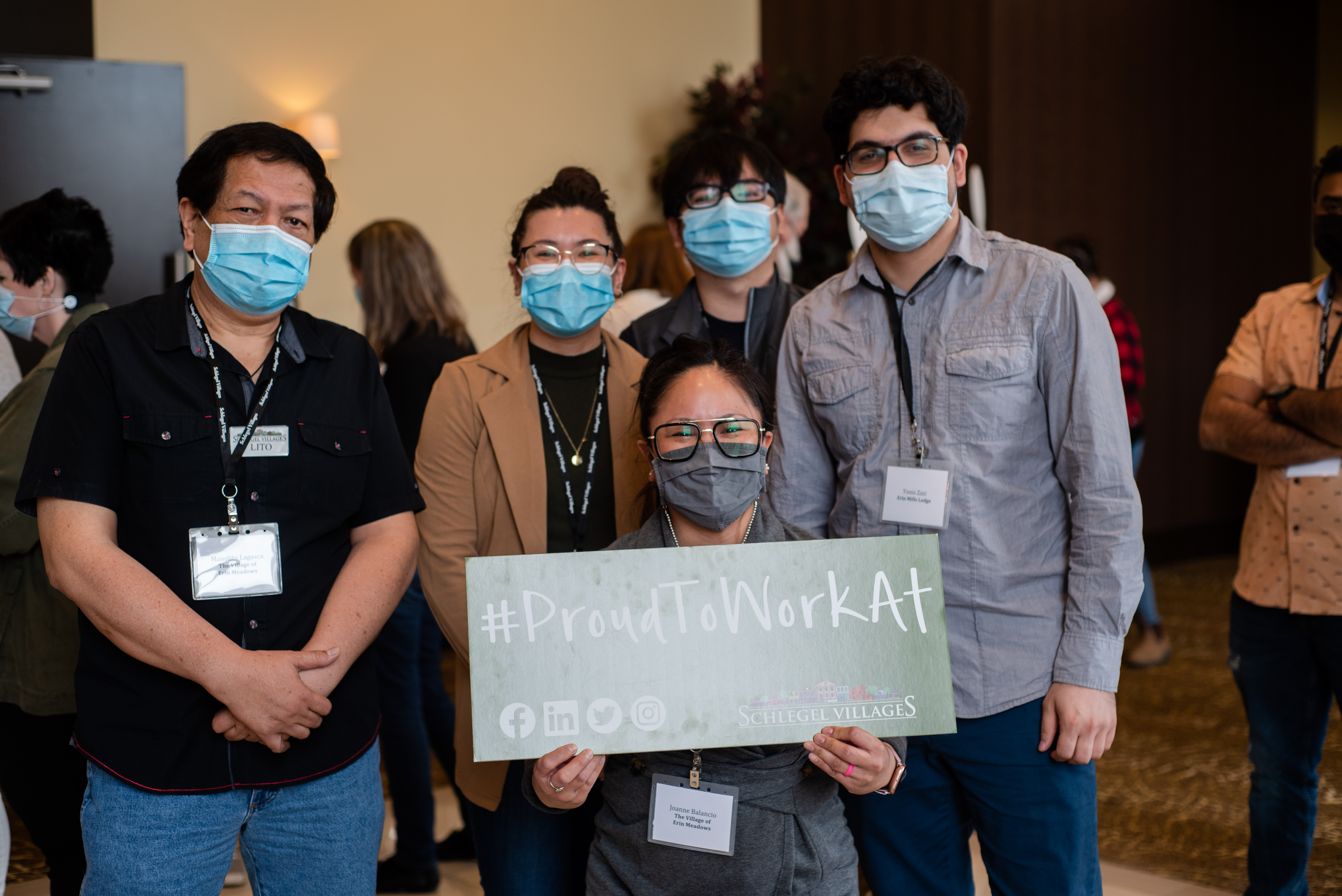
Canadians take pride in the publicly funded health care system, Dr. Bell said, knowing that the nearly 200 people in the room he addressed were proud to be some of the key players that make that system work. If this system is to be maintained, he added, then senior’s care and the innovations that will make it more cost effective are of critical importance.
Consider that today the province supports approximately 78,000 long-term care beds. Based upon the 3-5 per cent increase in demand the boomers represent, that number will reach more than 200,000 in the next 20 years.
“We have to think about ways to care for people differently, and it’s not just because we want to keep our system cost effective and sustainable and make sure the taxpayers can afford our system,” he said. “It’s also because that’s what Ontarians want and one of the great things about the Schlegel philosophy that I’ve seen is the opportunity for people to experience a continuum of care.”
Dr. Bell went on to explain that the province has made great strides in many areas; globally, in terms of acute care issues such as cancer care or kidney failure or hip and knee replacements, Ontario is a strong performer. Where we’re falling behind, however, is in the “retail” part of the system – primary care, mental health and addiction services or home care, for example.
He later offered the example of Eve, a hypothetical woman in her mid-80’s who represents the type of person the people gathered in the room are best-suited to support.
Four years ago, Eve lost her husband. She still lives in the home they bought together nearly 60 years before. Every throw rug represents a memory, but also a fall hazard. The home is no longer safe for Eve, but she fails to see the threats or perhaps ignores them. One day she falls, breaking her hip – the story is familiar to everyone in the room as Dr. Bell describes the situation, and everyone in the system knows just how dangerous this is for Eve.
She gets to the operating room within 24 hours, but even the best hospital in the world is a dangerous place for Eve. She’s suffering incredible pain and starting to become confused from the painkillers. She develops pneumonia and full-blown delirium. She’s been in bed for the past ten days and there’s significant muscle decline because of the lack of nutrition and the opioids she’s taking to handle the pain.
“This woman, who at the age of 86 was utterly independent and required no health services except visiting her doctor once in a while . . . suddenly she has fallen off a cliff,” Dr. Bell says. “It wasn’t a stairway she fell down, she just fell off an independence cliff.”
There is a lot going against Eve in today’s system, Dr. Bell explained, and getting her back to the point of independence, which is everyone’s ultimate goal, is extremely difficult within an acute system that isn’t designed to meet her needs.
Dr. Bell then looks to the innovators in a room filled with direct care partners, long-term care leaders, residents, family members and the researchers who seek answers to some of the great challenges facing the aging population, and he asks: “What does Eve need?”
Continued in the next Village Voice . . .
- Previous
- View All News
- Next