PERT Team enhances their understanding of the well-being of those they support
By Kristian Partington
A comprehensive dementia support program isn’t created overnight; there isn’t a one-stop binder a caregiver can download or a long-term care organization can purchase to help them better understand the lives of those they support. Layer upon layer of complementary approaches require ongoing education in order to create a new depth of understanding, and in an organization like Schlegel Villages, dedicated champions must help each layer spread to all residents, team members, families and community partners.
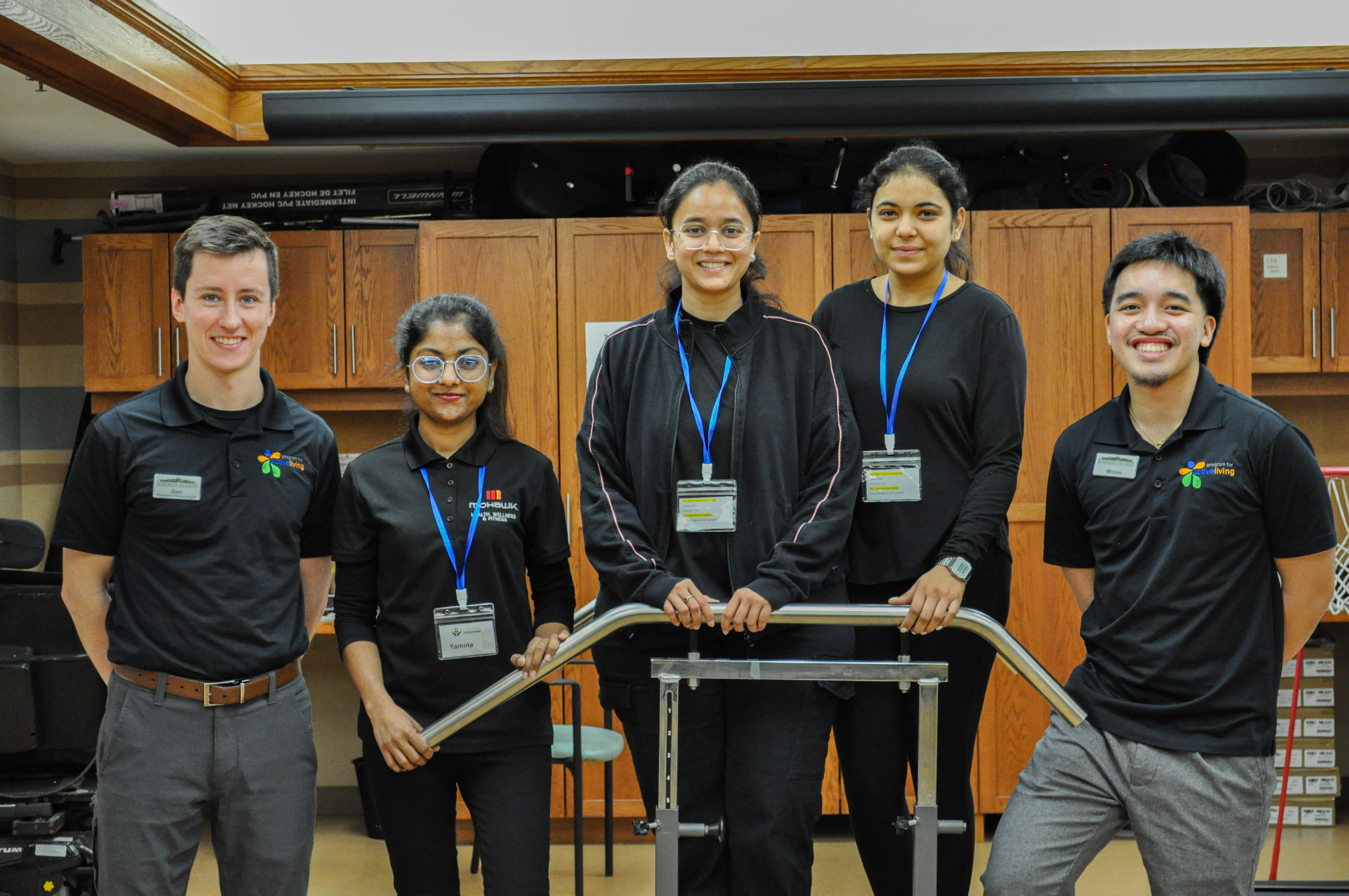
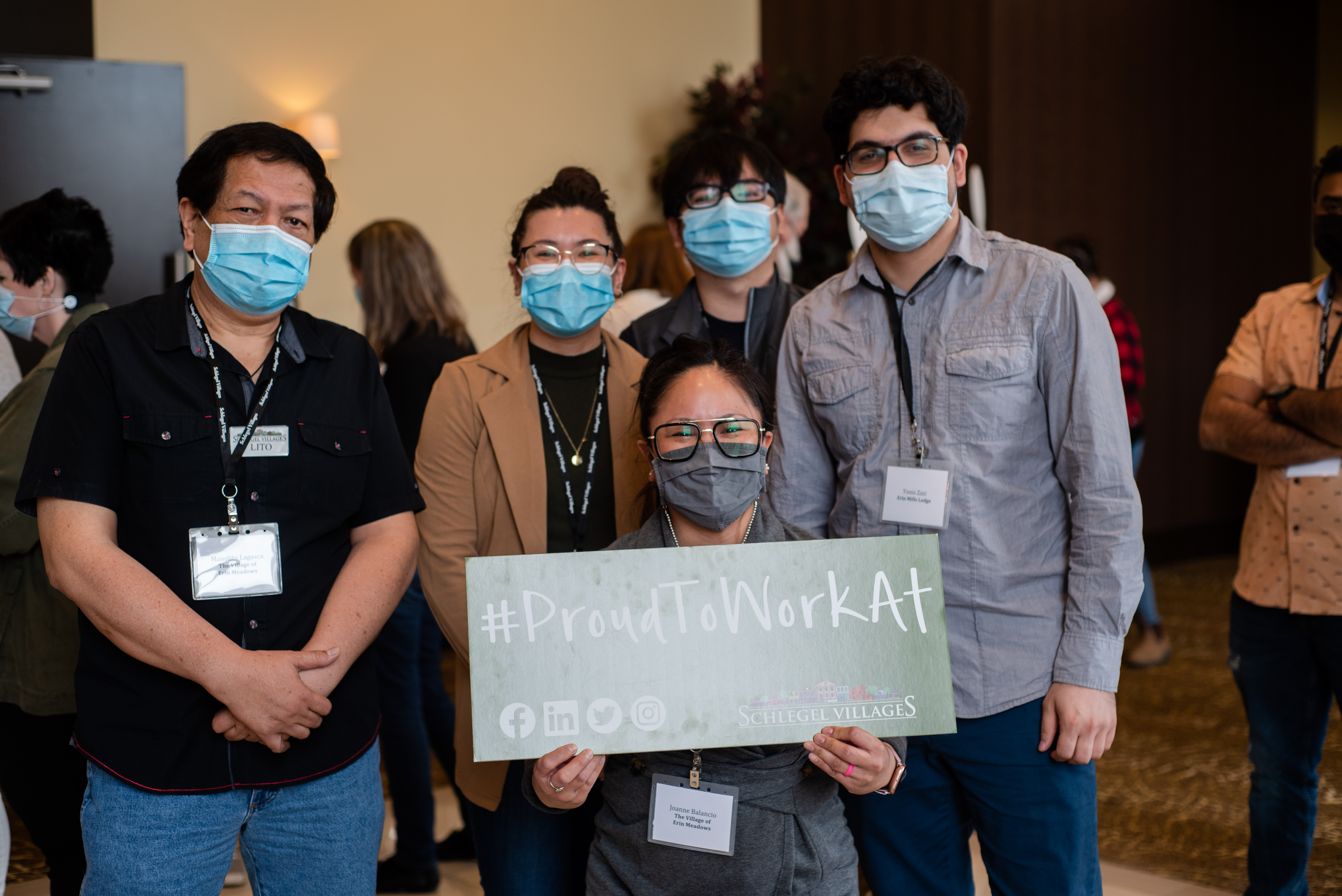
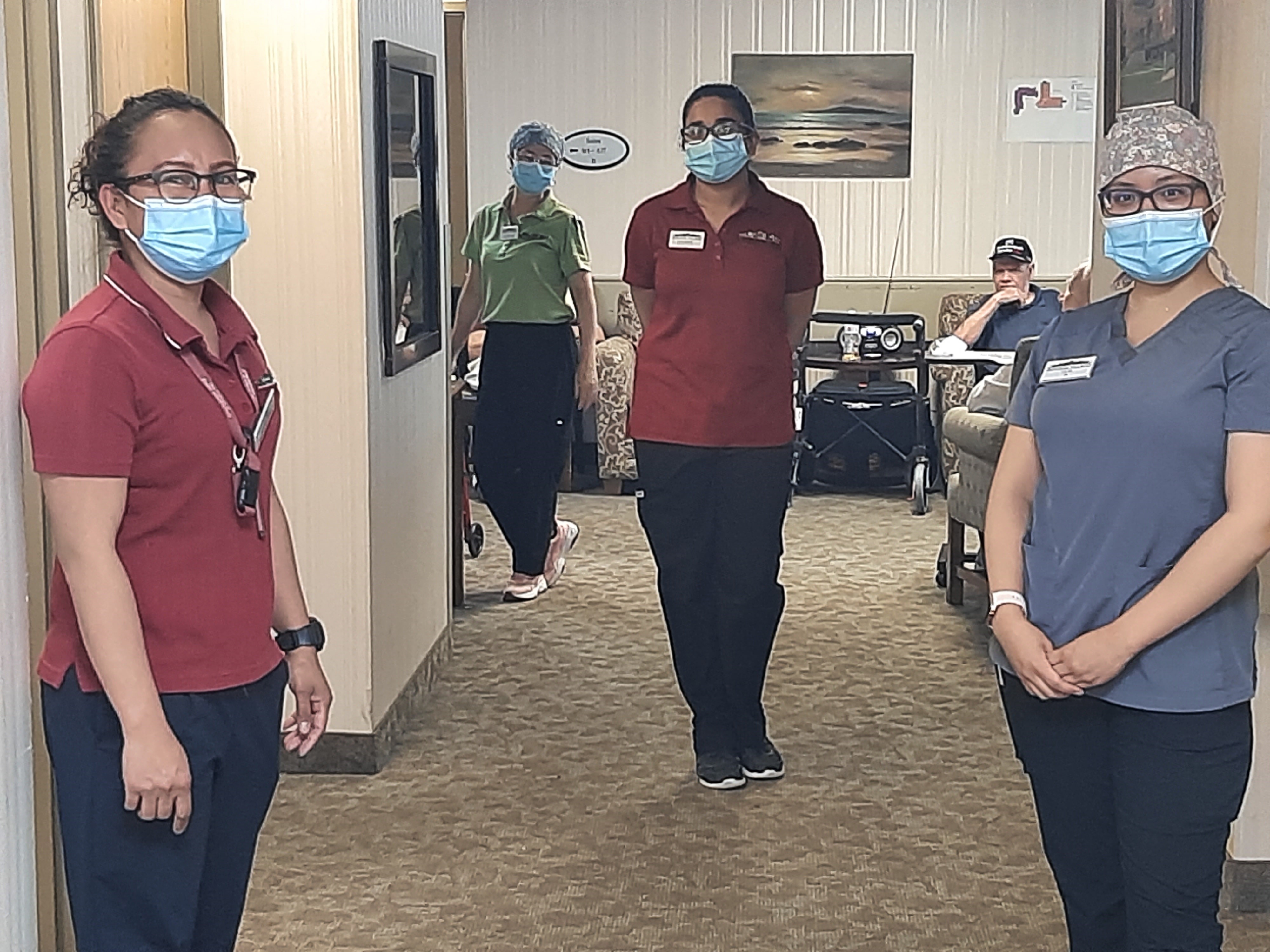
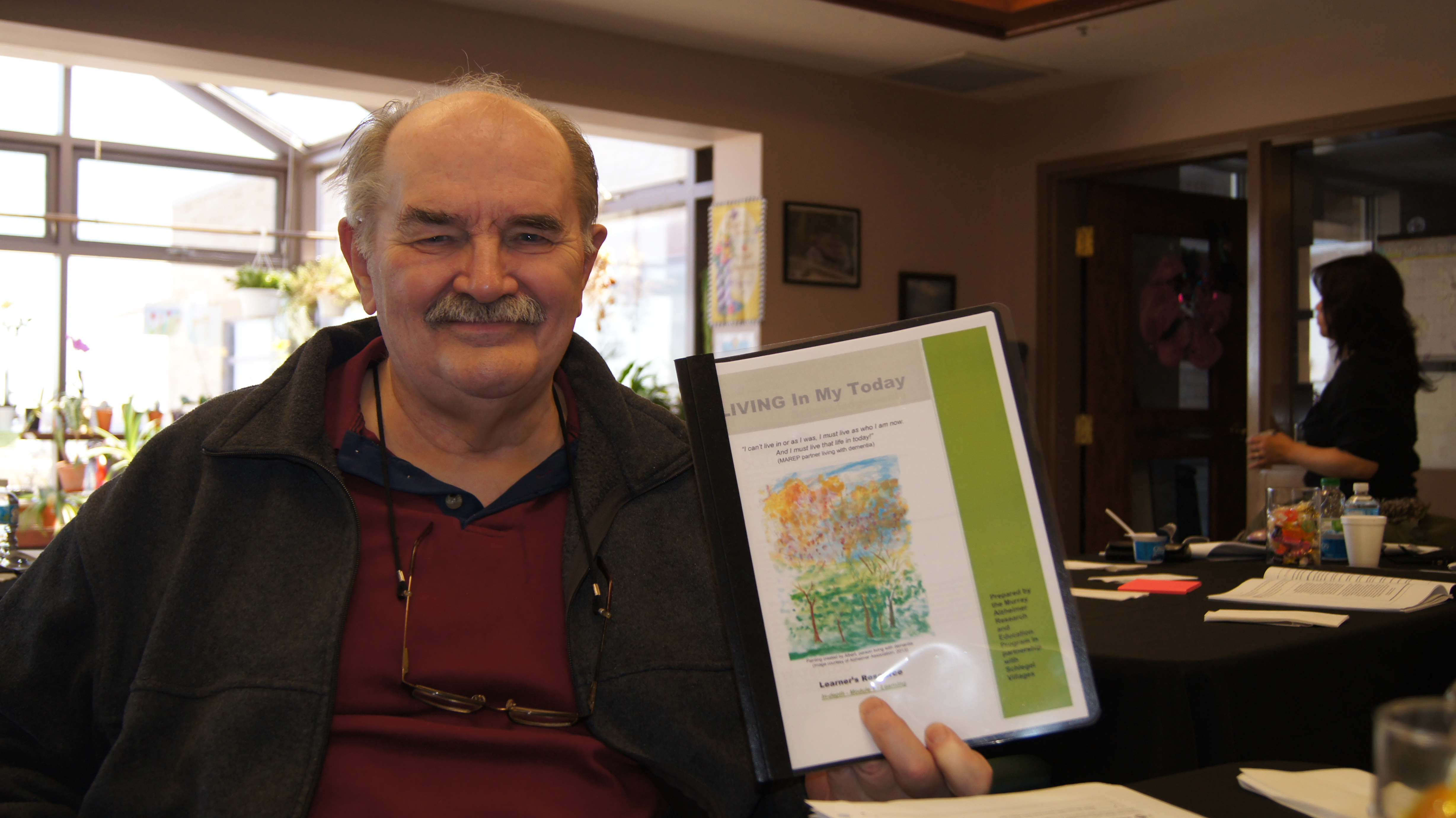
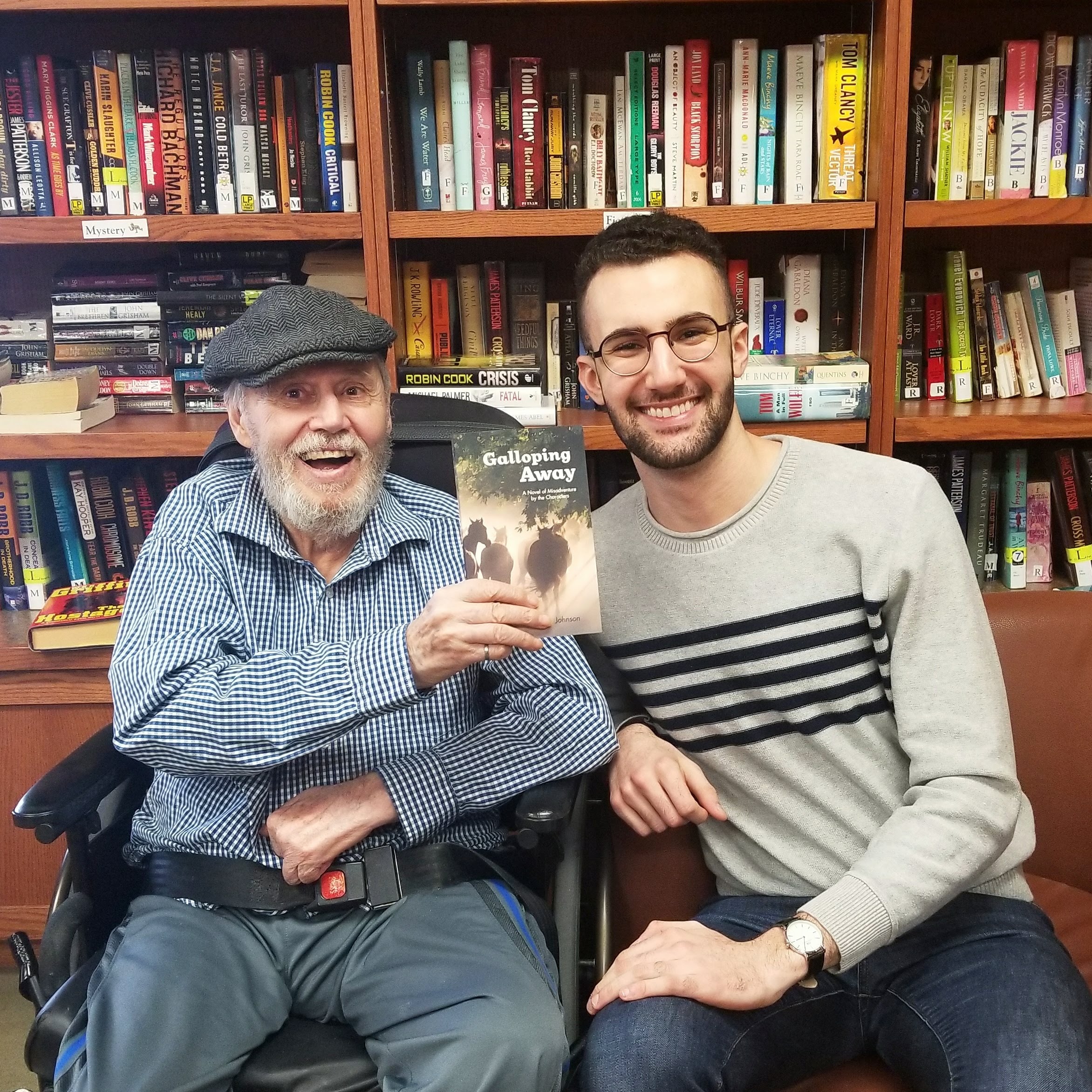
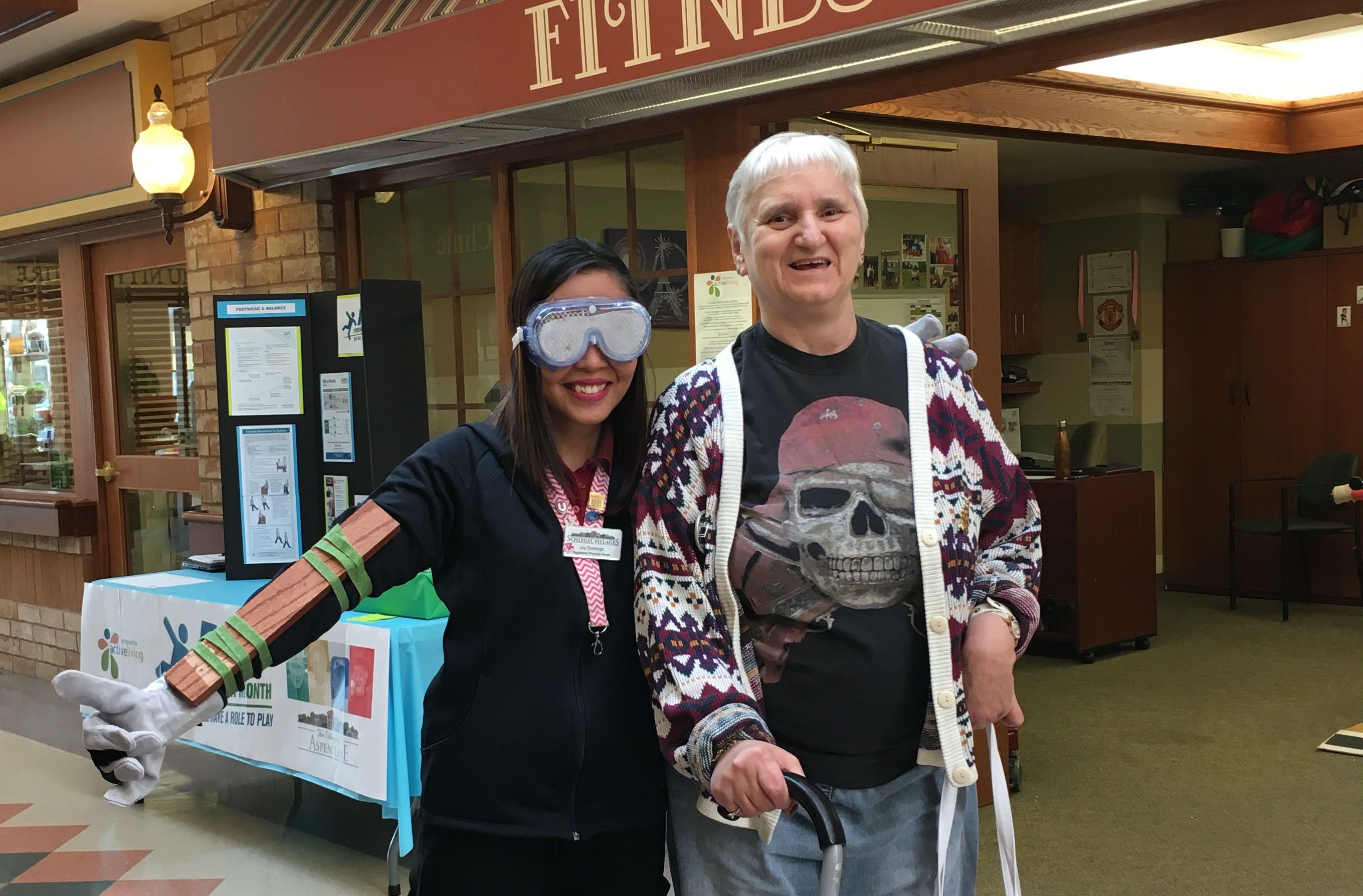
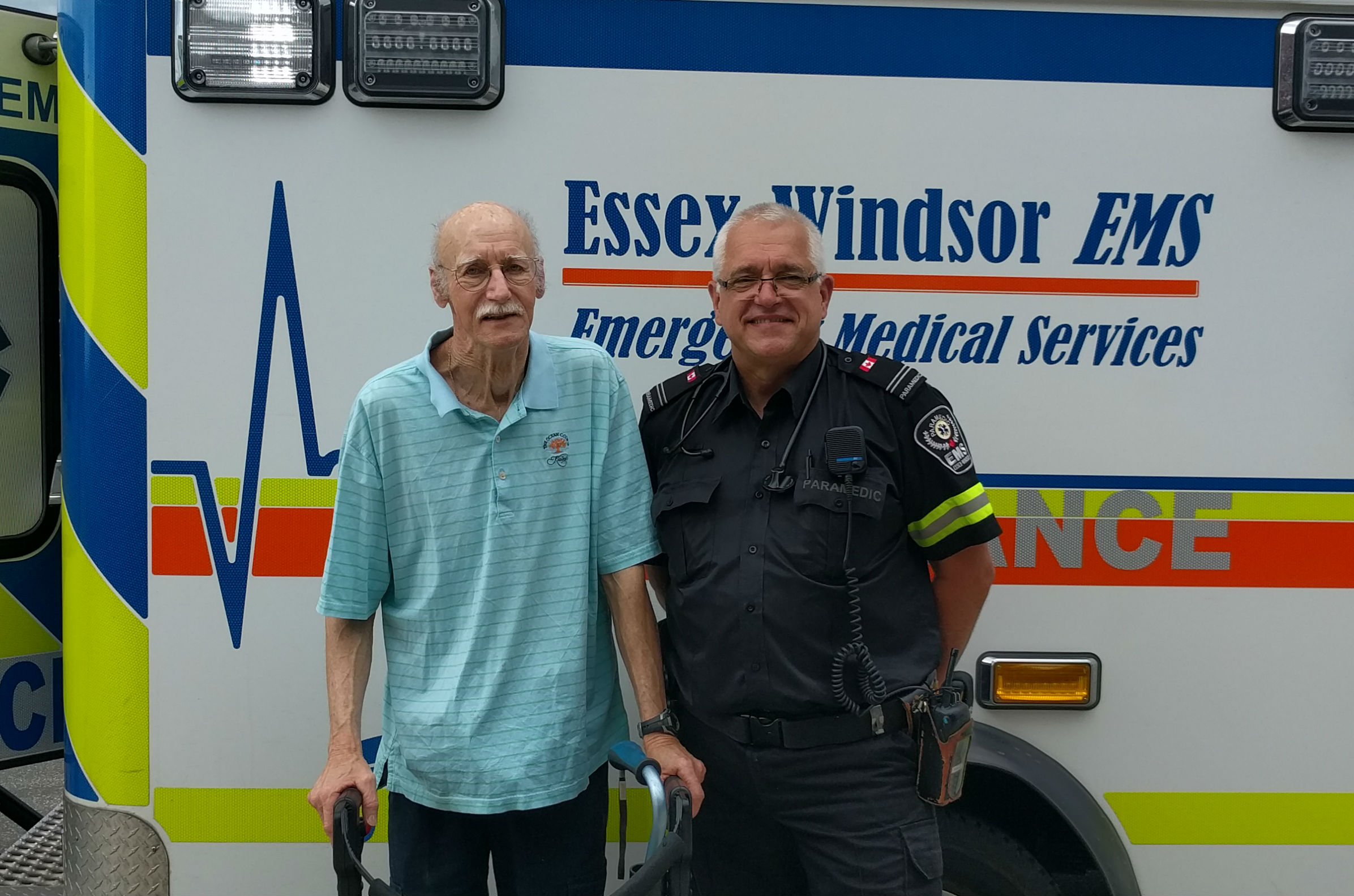
On Jan. 10, a core group of these champions gathered at the Village of Arbour Trails in Guelph for their semi-annual meeting. These are the members of the Personal Expression Resource Team (PERT), which for more than two years has been inspiring new approaches to support for people living with dementia, especially those who express themselves in challenging ways. The team and its individual members within the villages are key aspects of the Schlegel Villages Dementia Care Program, and when placed in tandem with concepts like the Layered Natured Framework and the LIVING the Dementia Journey education program, the PERT approach can have great benefits.
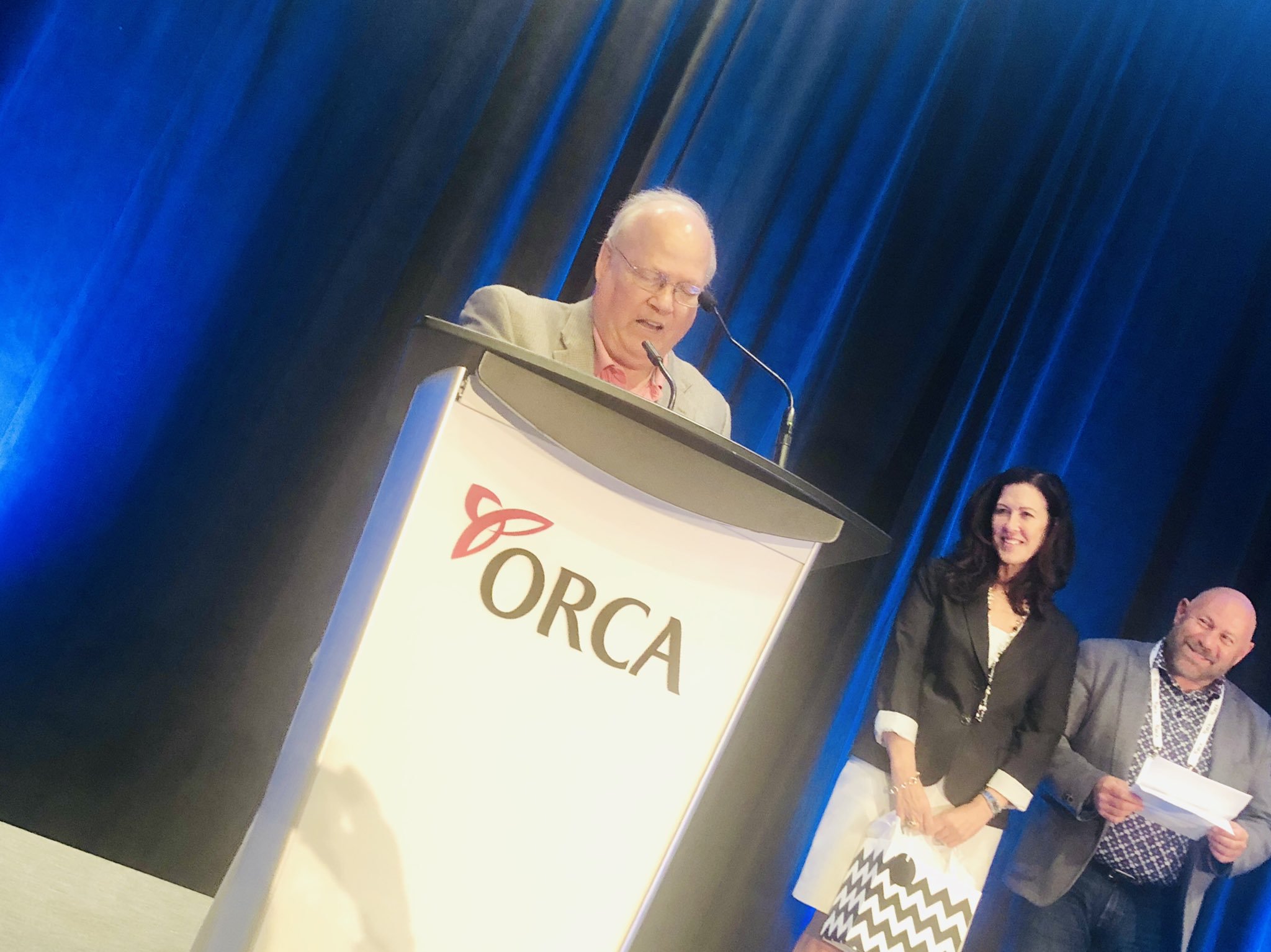
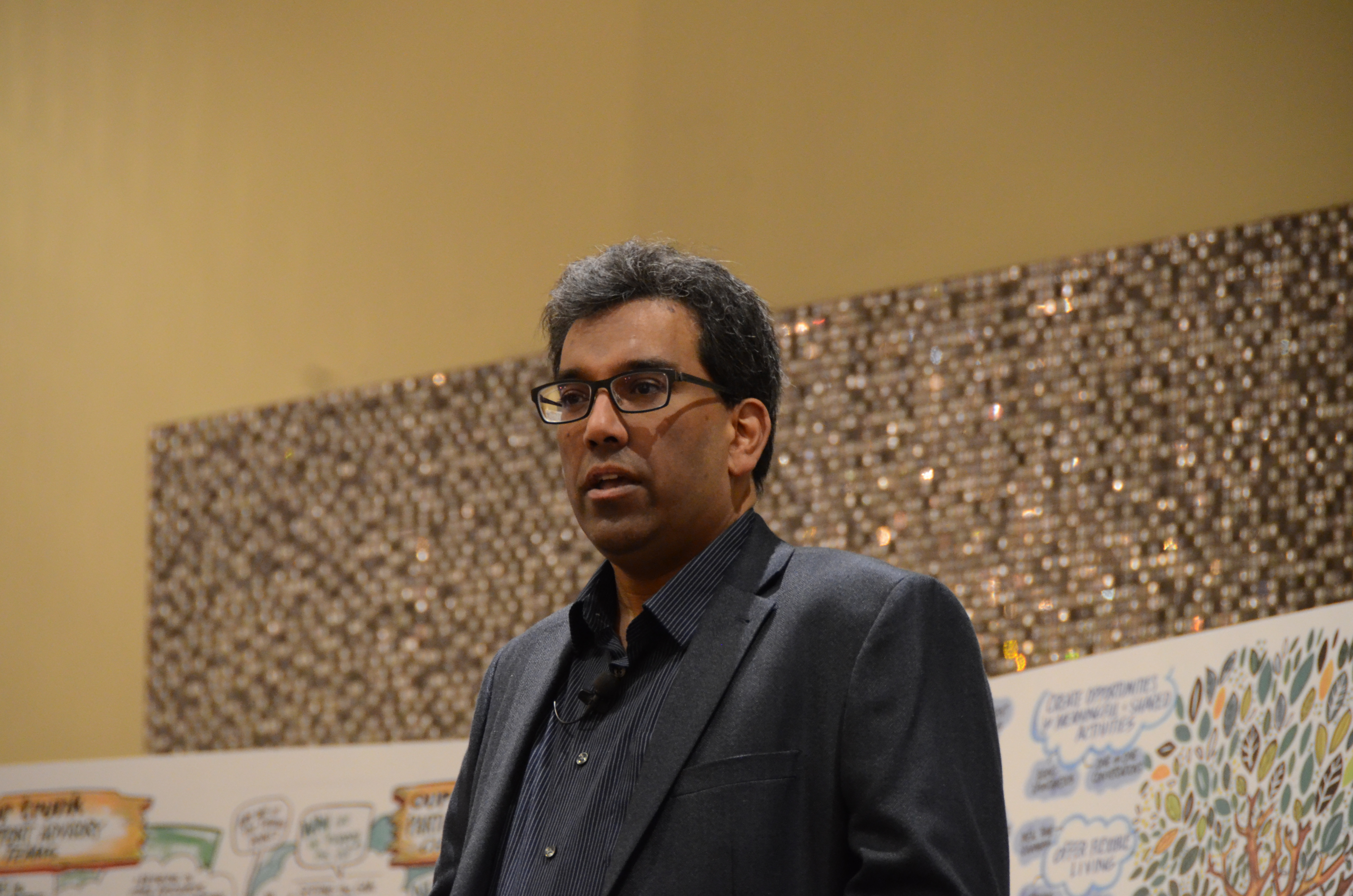
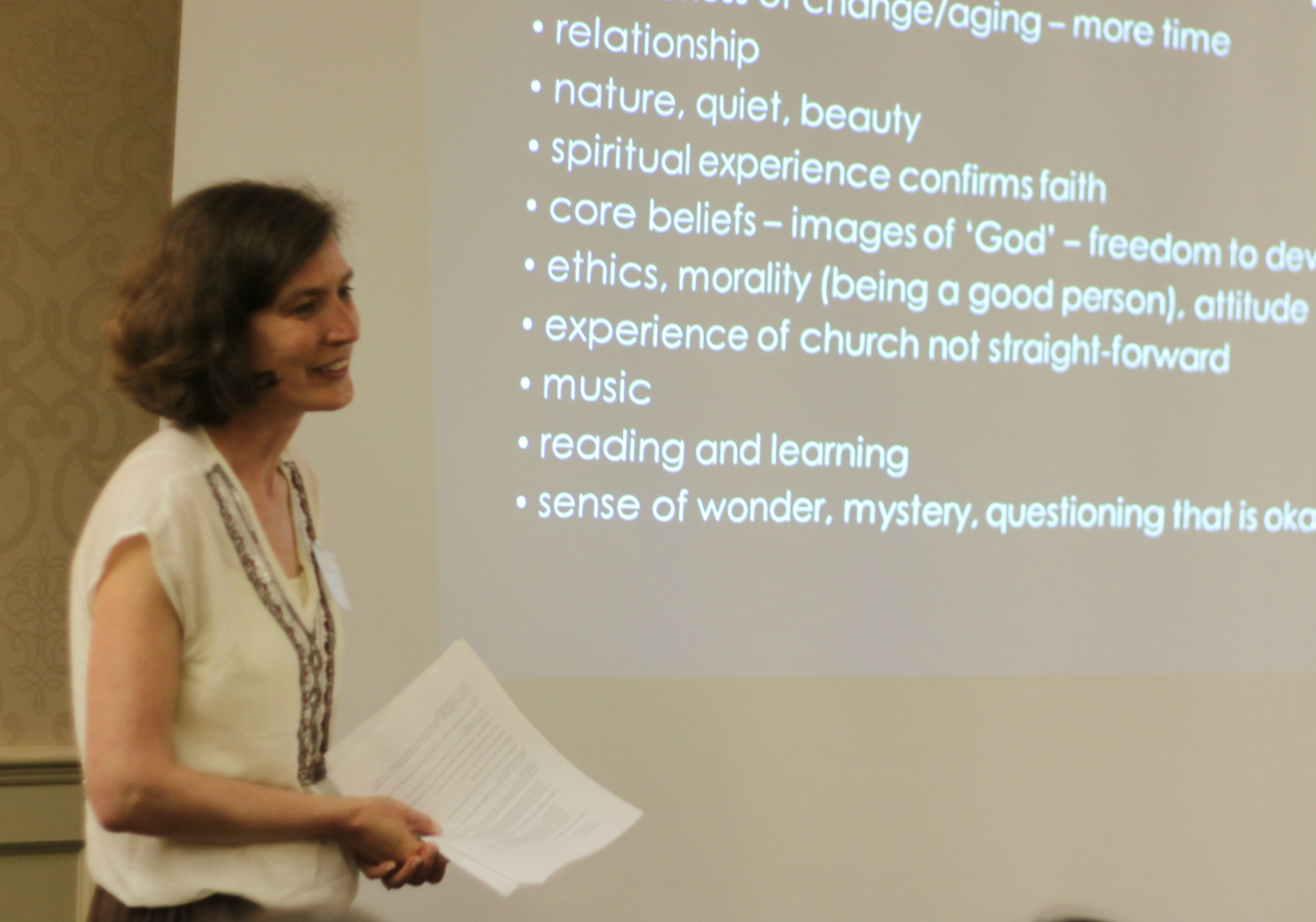
Author, educator and geriatrician Dr. Allen Power opened the day with a condensed version of his typical two-day seminar discussing the unnecessary prevalence of anti-psychotic medications among people living with dementia. Al, who has been working closely with Schlegel Villages this past year to strengthen the dementia care program, told the group that in almost all cases, people living with dementia express themselves in challenging ways because something important is missing in their lives – something a pill can not replace.
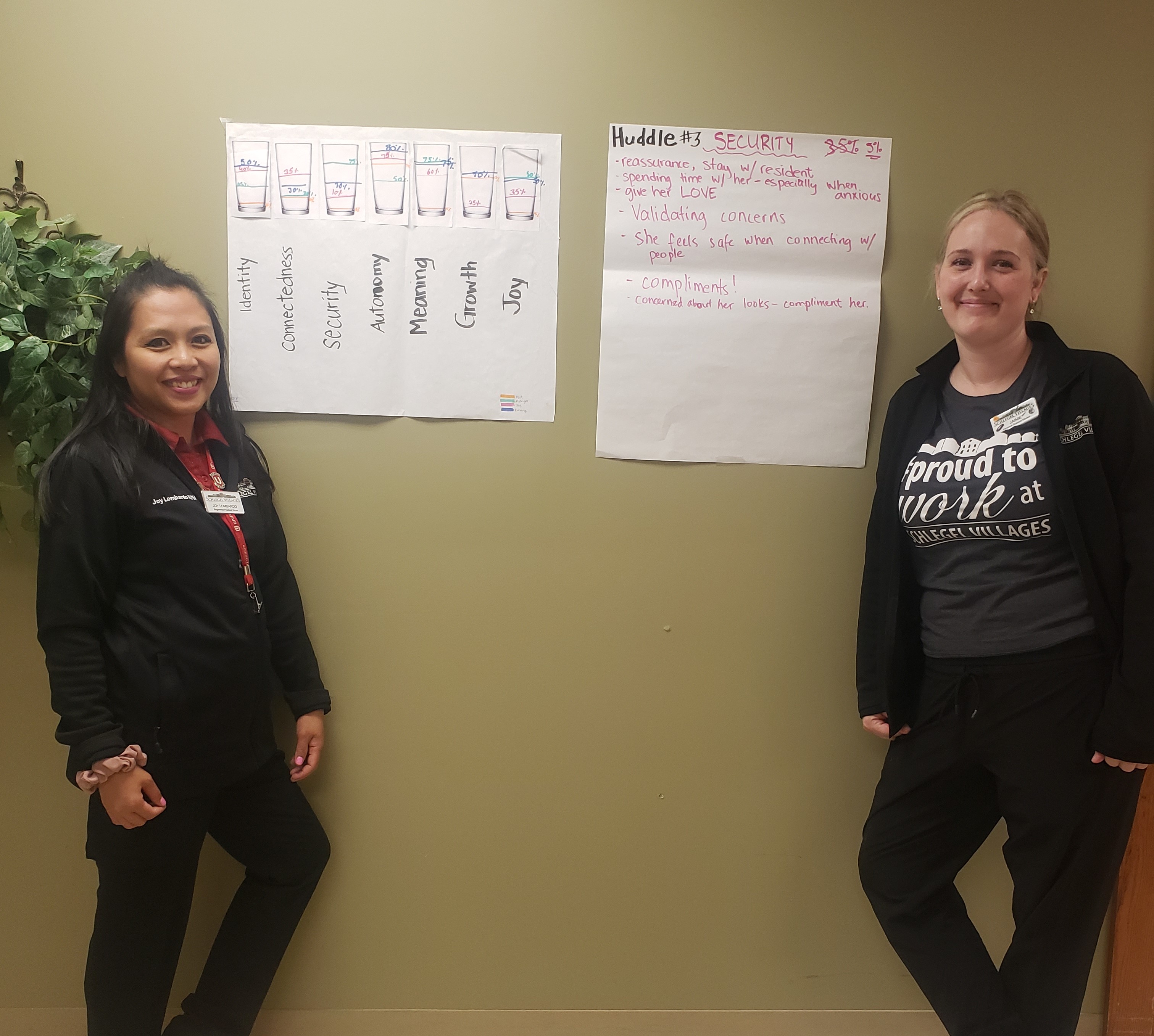
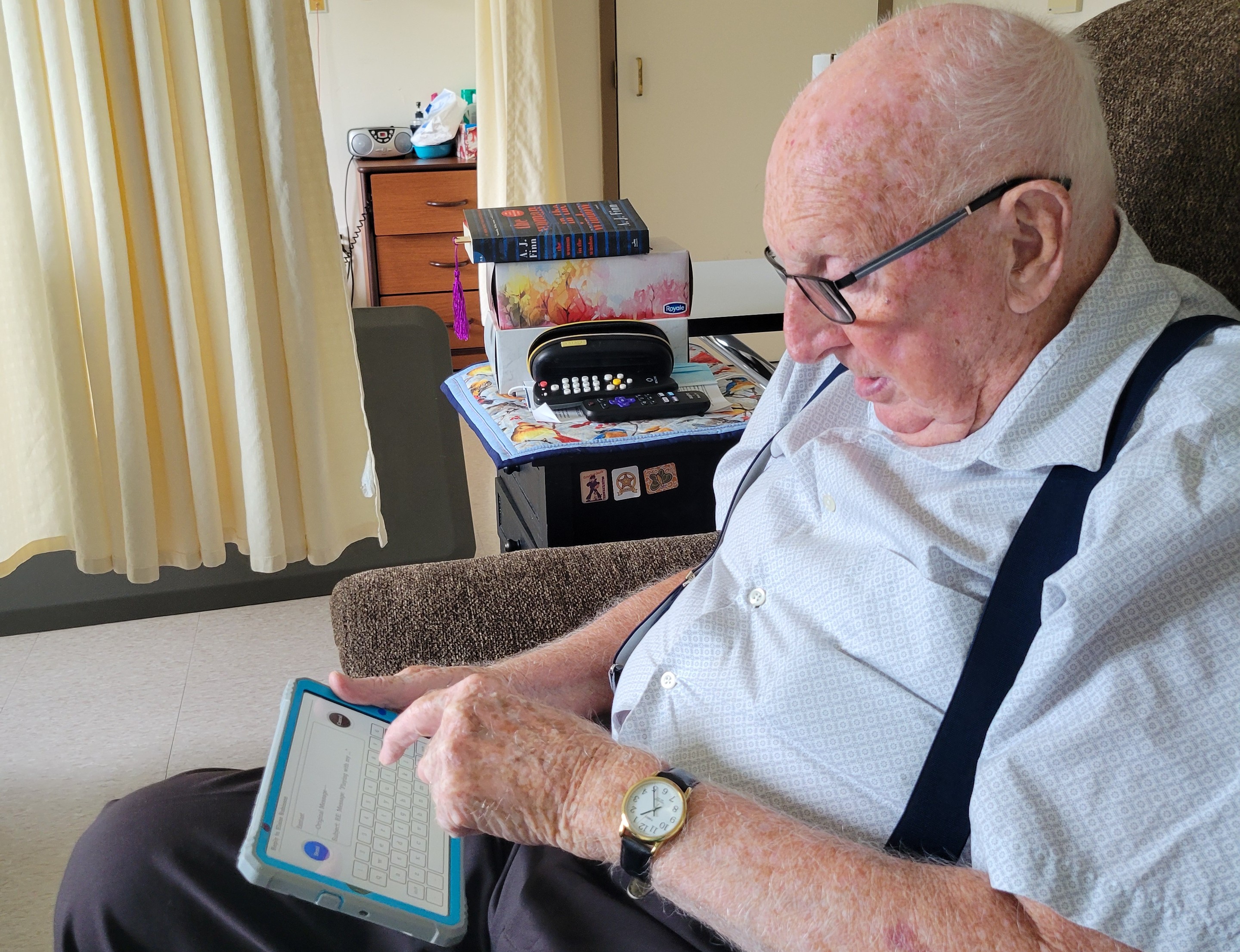
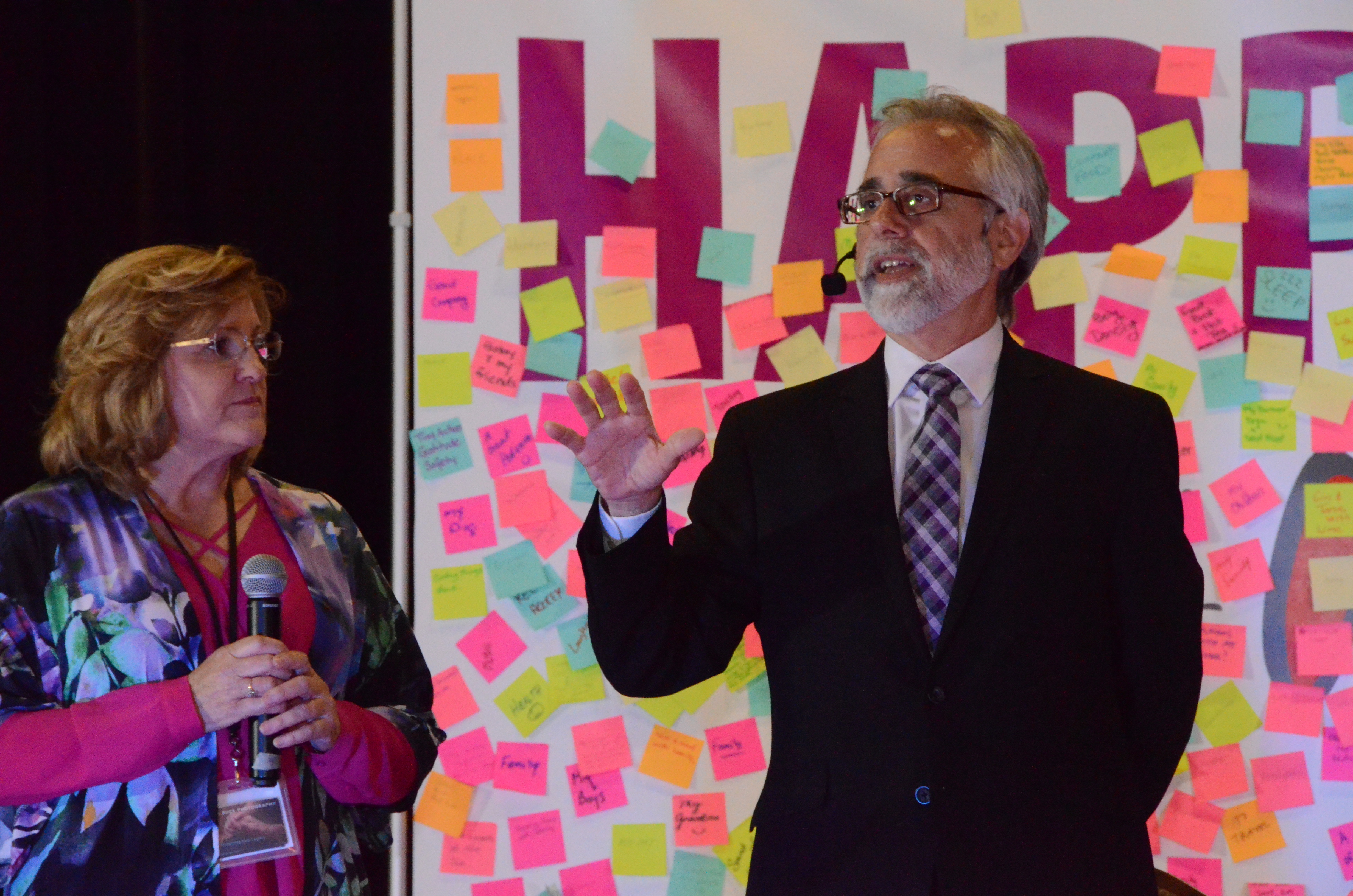
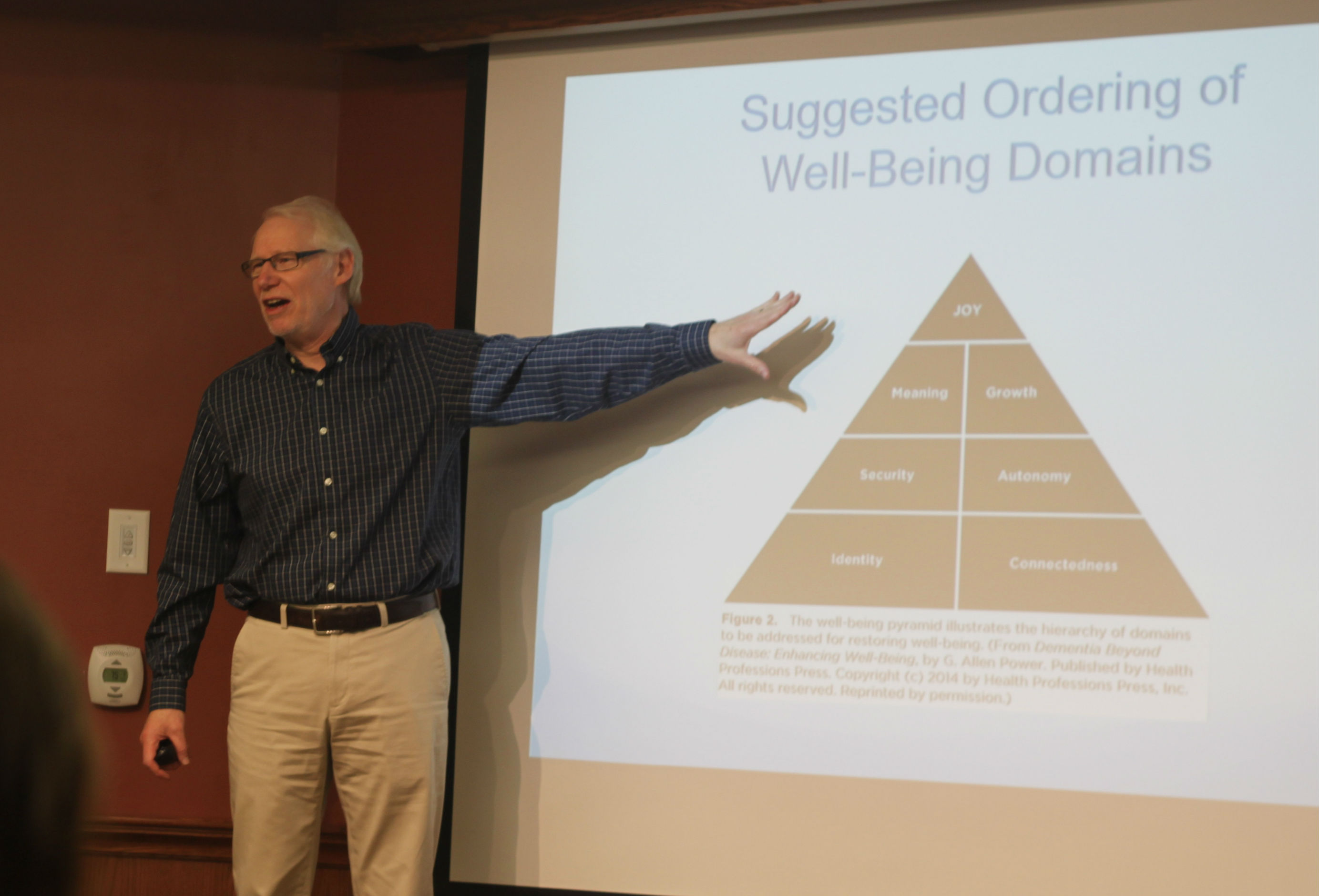
“Antipsychotics are largely ineffective and they are dangerous,” Al says. “In fact, there is no chemical rationale for using antipsychotics other than sedation.” He urged the team to consider the concept of personal well-being from seven different domains: Joy; Growth; Connectedness; Security; Autonomy; Identity and Meaning. When someone, whether they have a dementia diagnosis or not, is lacking in one or more of these areas, they’re life is less than fulfilled and they may express that through various emotions, such as anger or sadness. The true problem comes when people strive to treat these emotional expressions with medication when perhaps what is really needed is a better sense of security or a deeper feeling of connectedness or autonomy.
“How long could I live in a place where alarms were going off 24/7?” Al questioned. “How long could I live in a place where people were telling me what to do all day and I had no input before I would get frustrated?
“It’s not rocket science,” he adds. “Sometimes the things that upset people living with dementia are the things that would upset all of us, so how can we connect that knowledge to understanding better ways to support them in spite of the difficulties they have?”
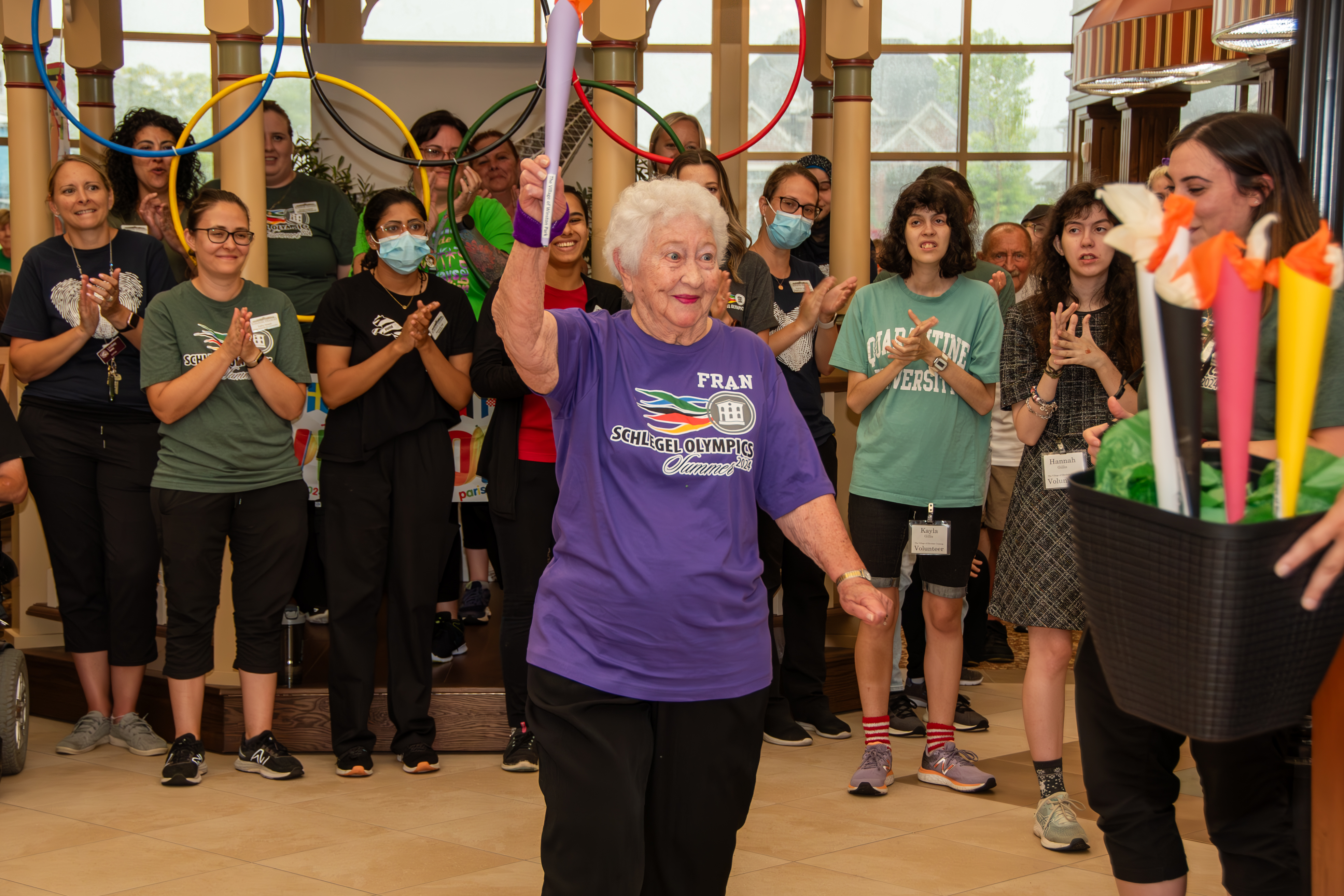
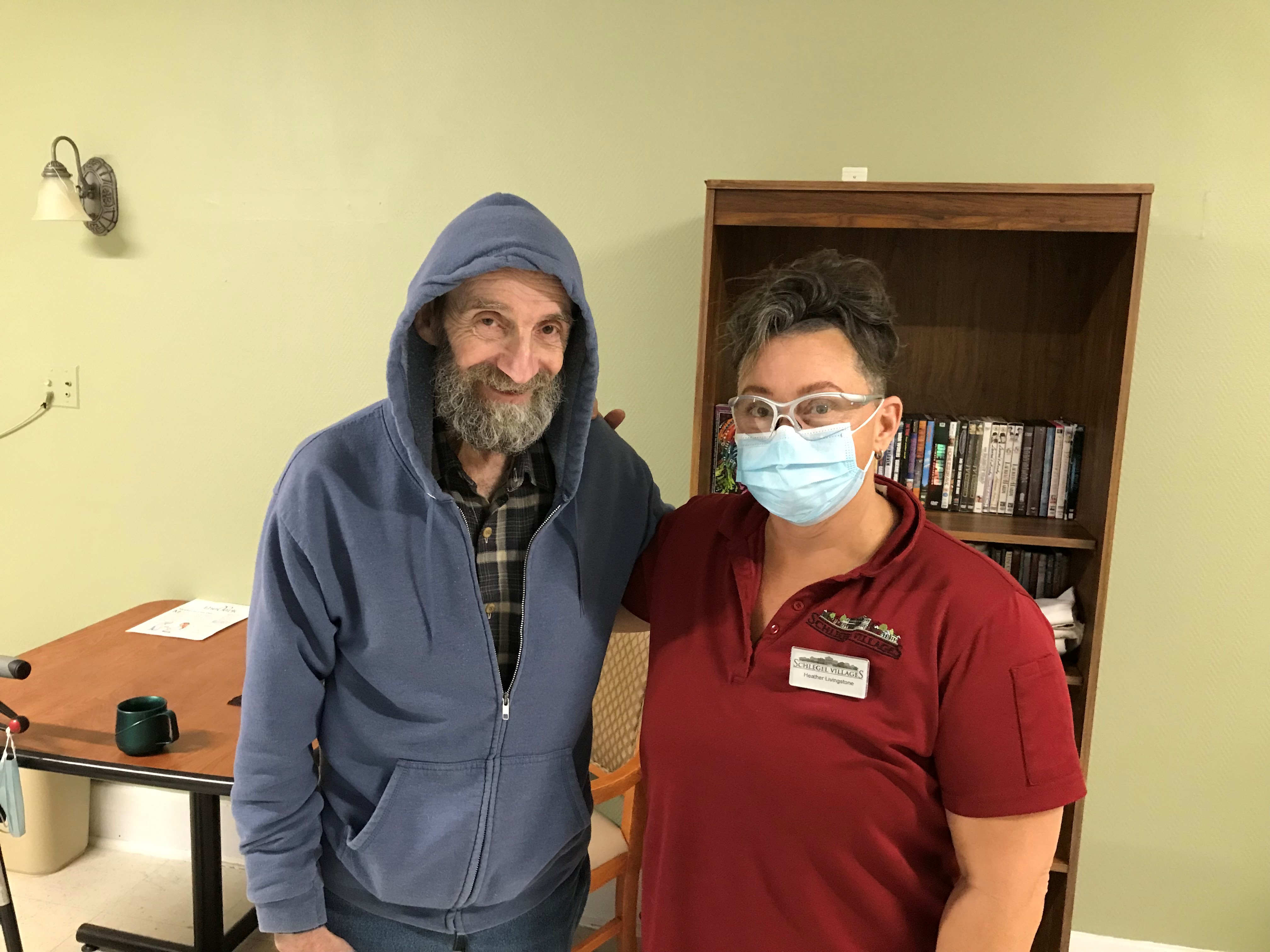
True support for any resident within the villages is about offering opportunities for the enhancement of personal well-being and this is no different where dementia is concerted. As advocates, the PERT team understands this and will continue to spread this understanding throughout their villages adding a deeper layer of depth to the overall Schlegel Villages dementia-care philosophy.
- Previous
- View All News
- Next