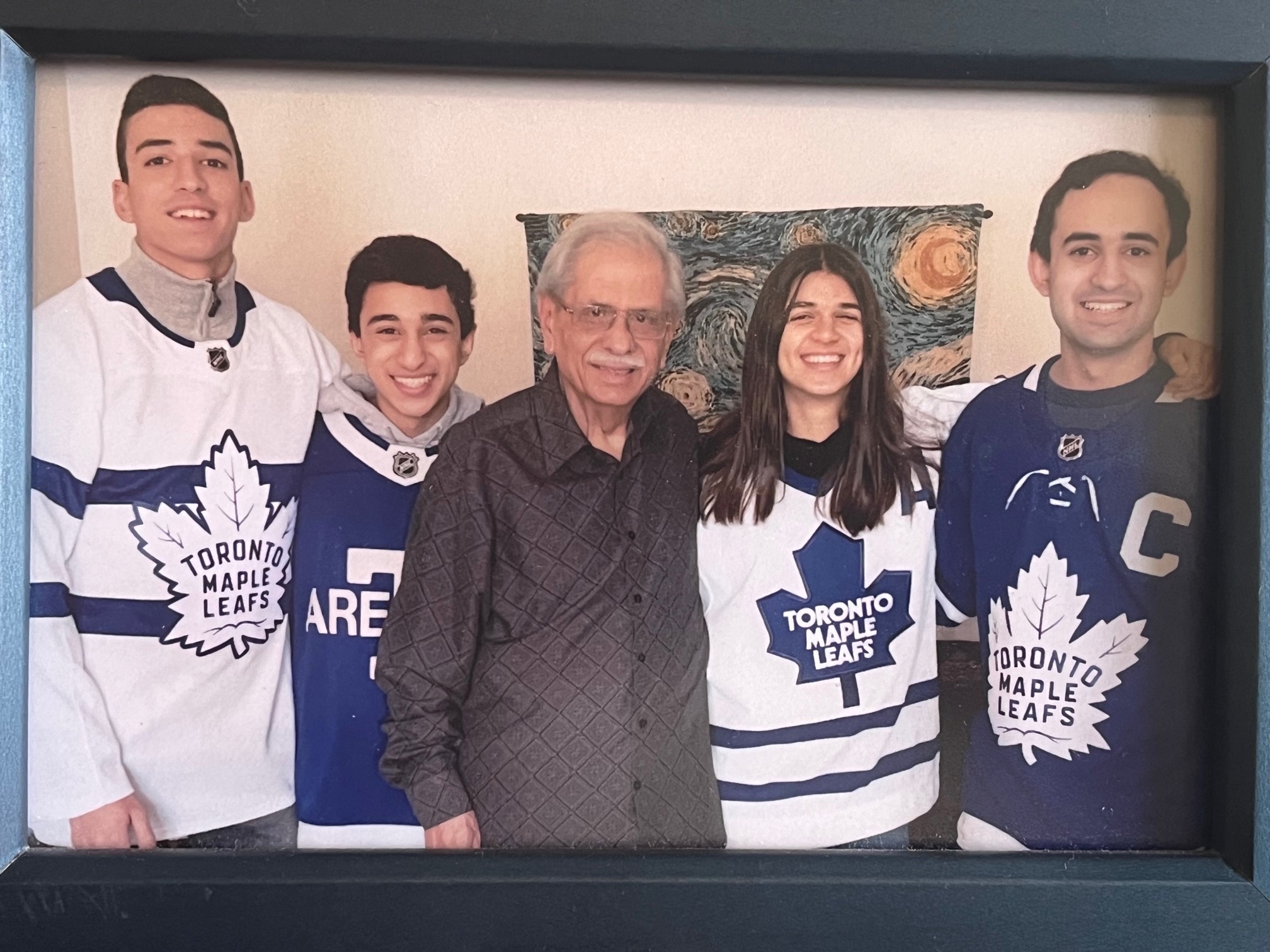
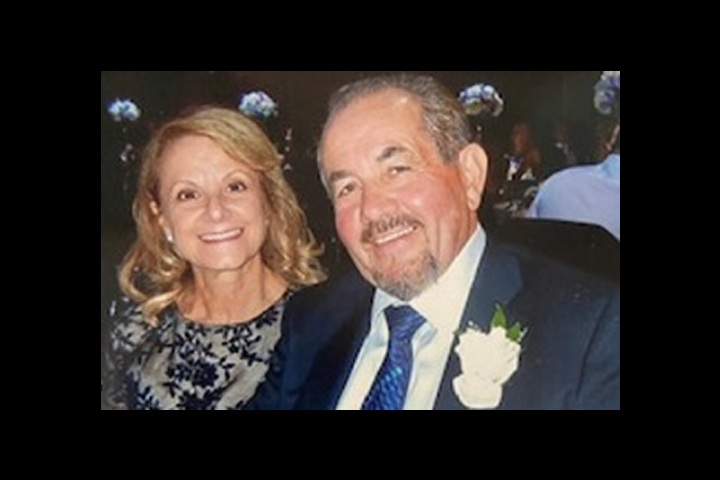
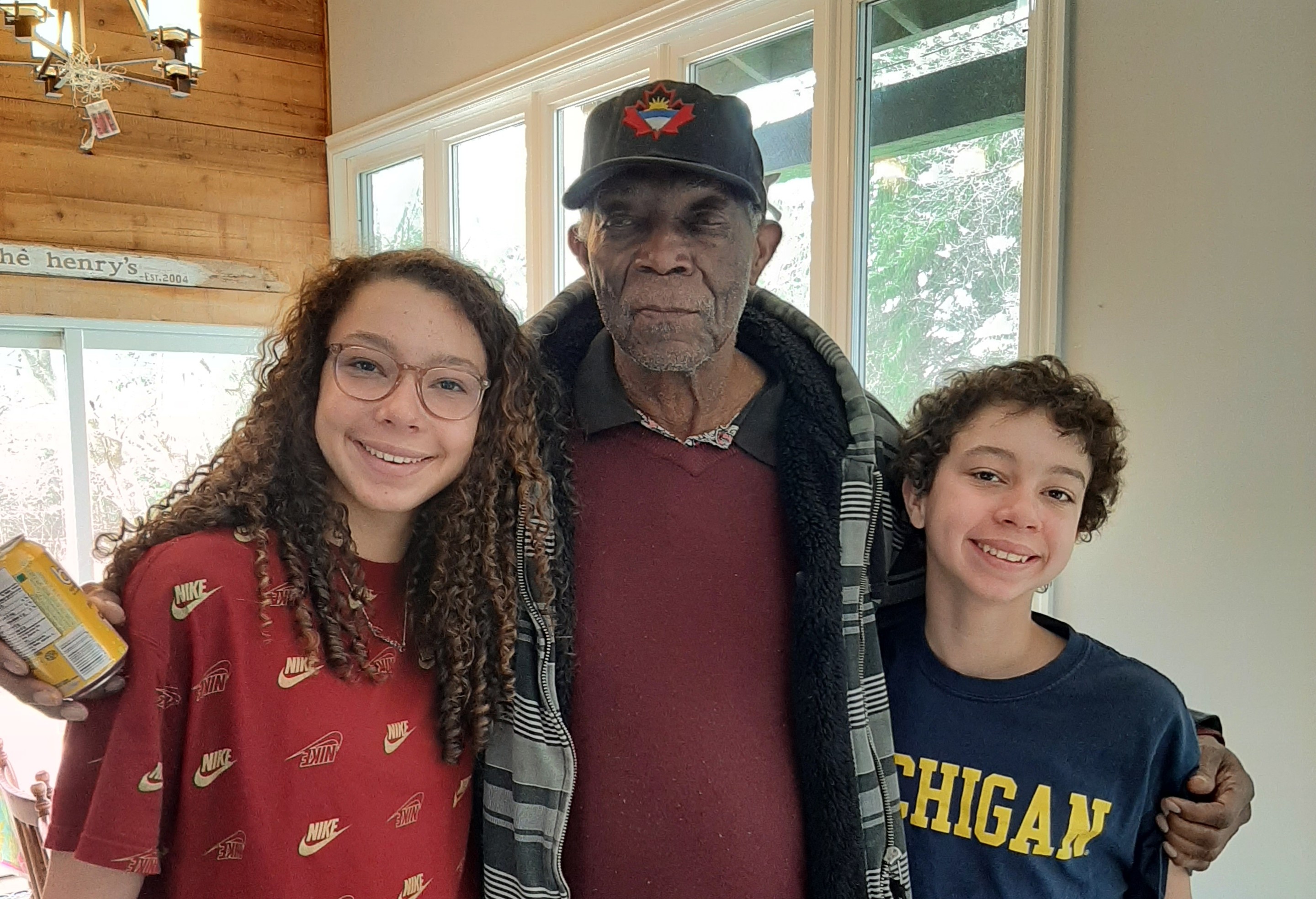
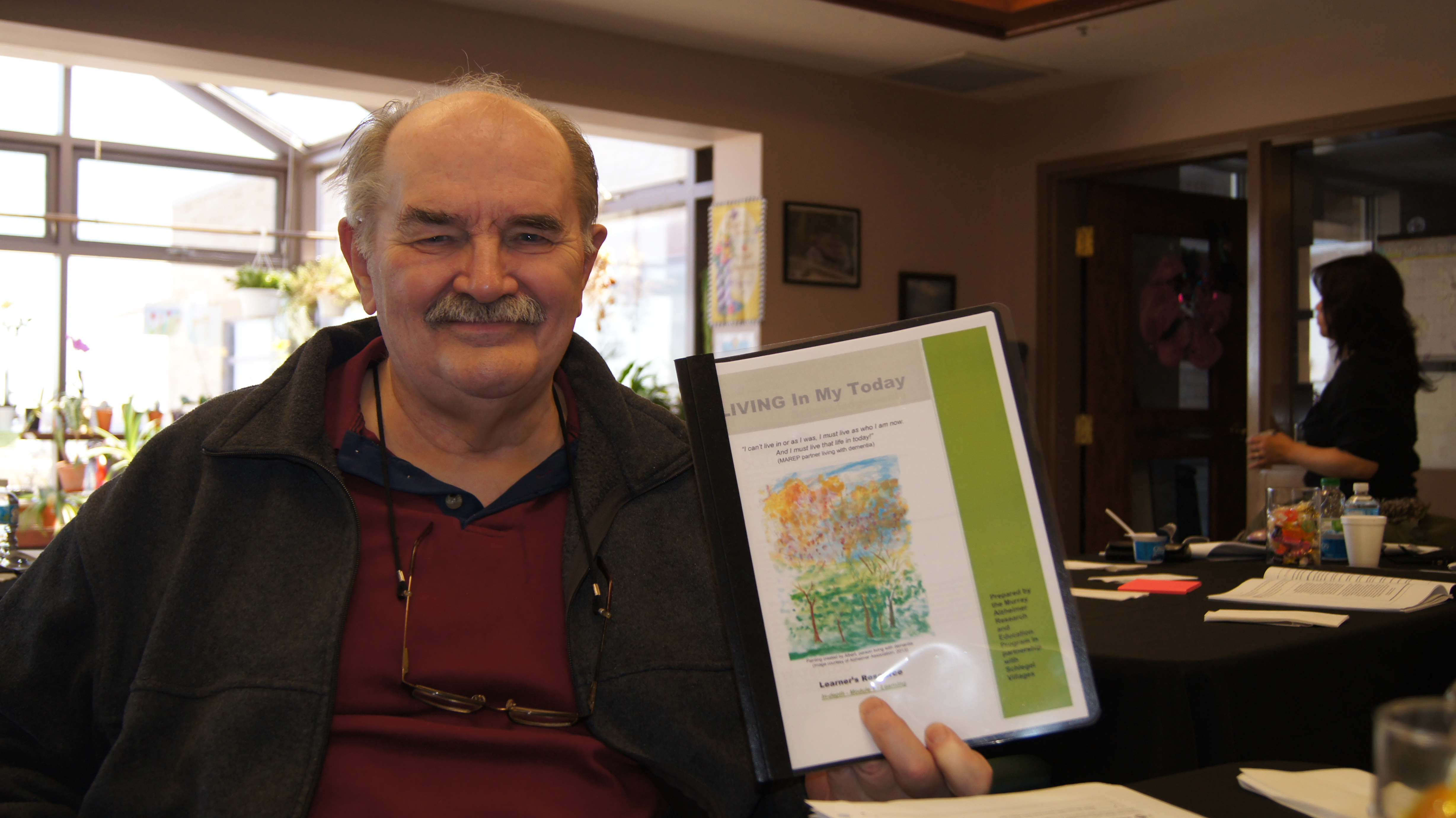
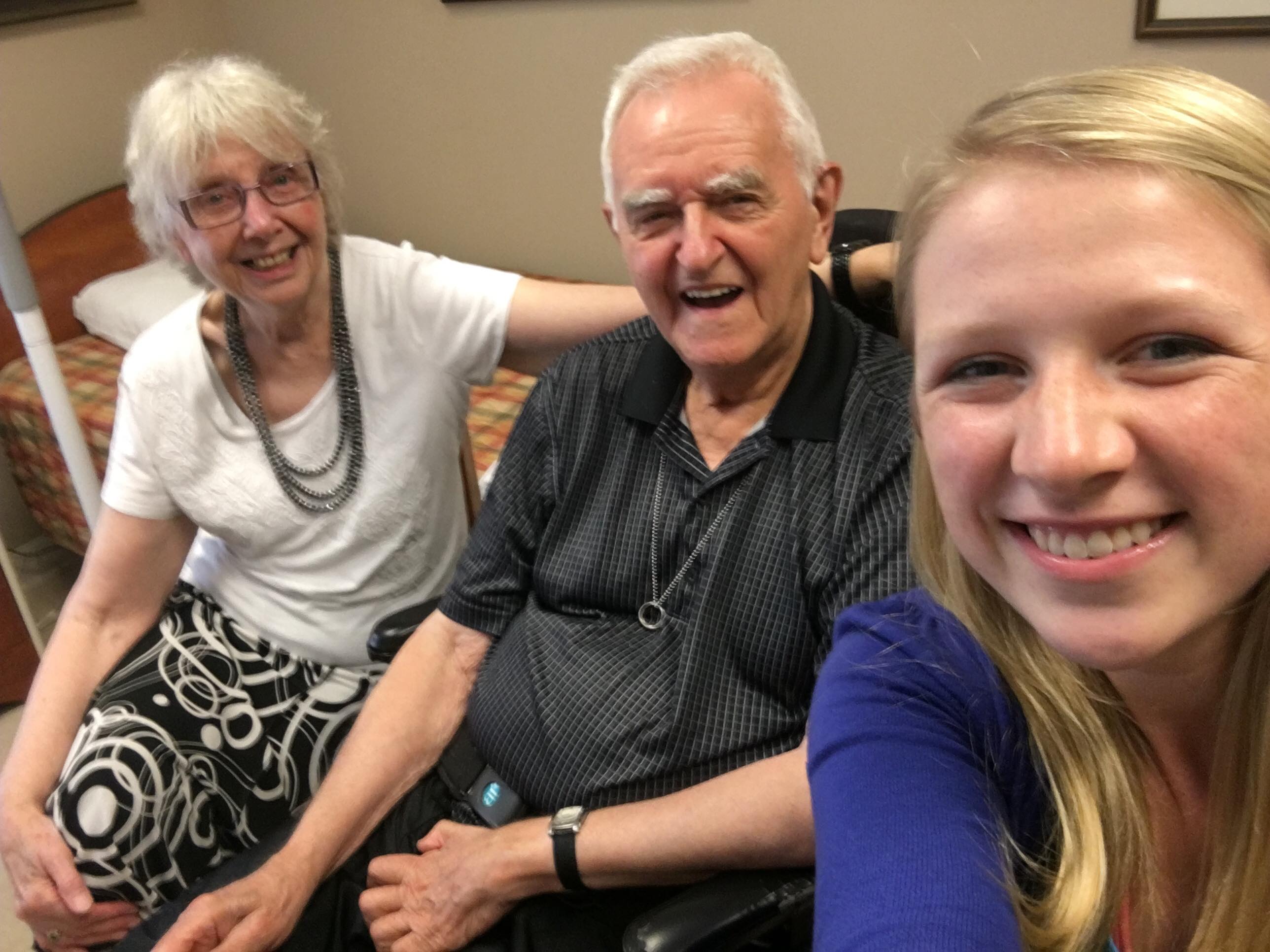
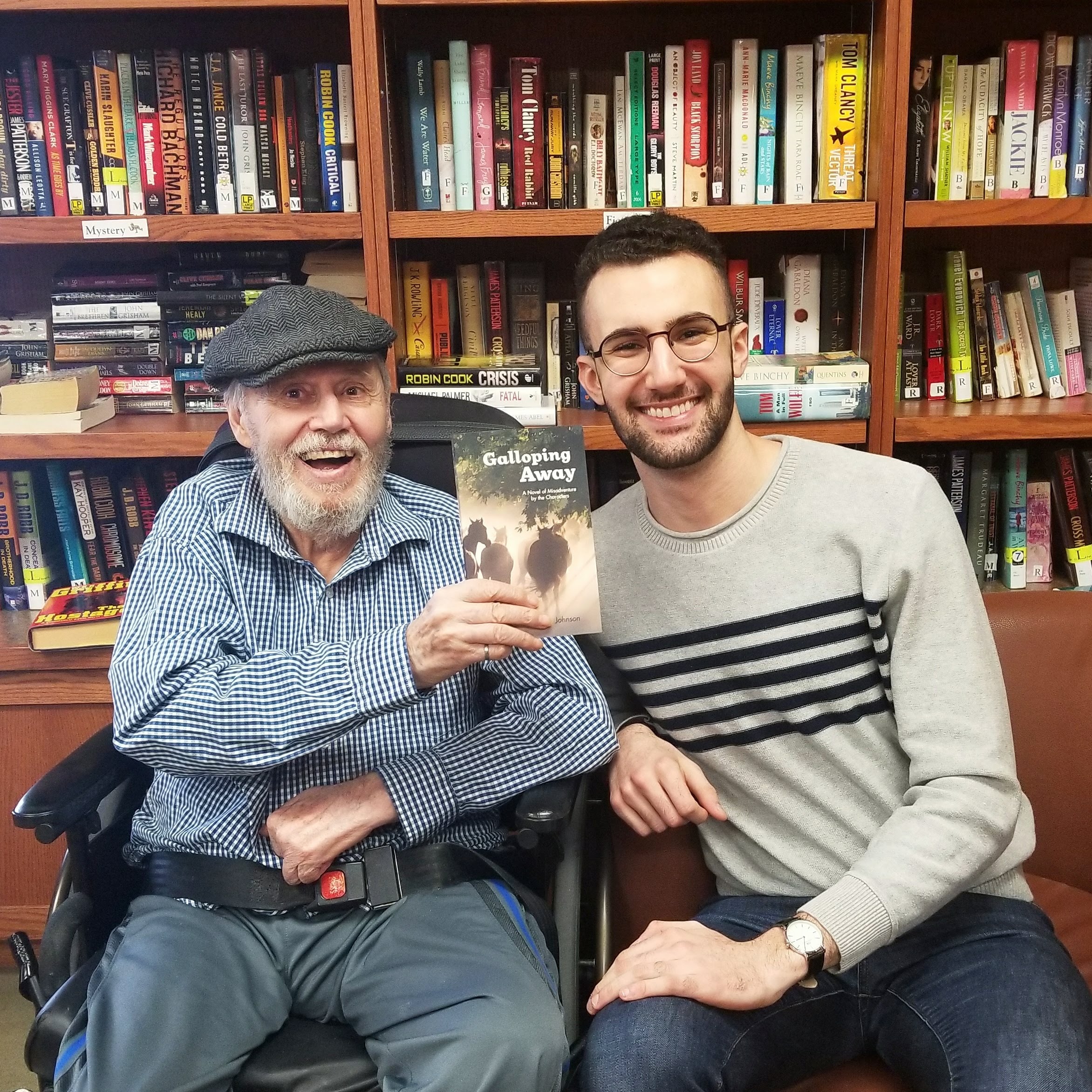
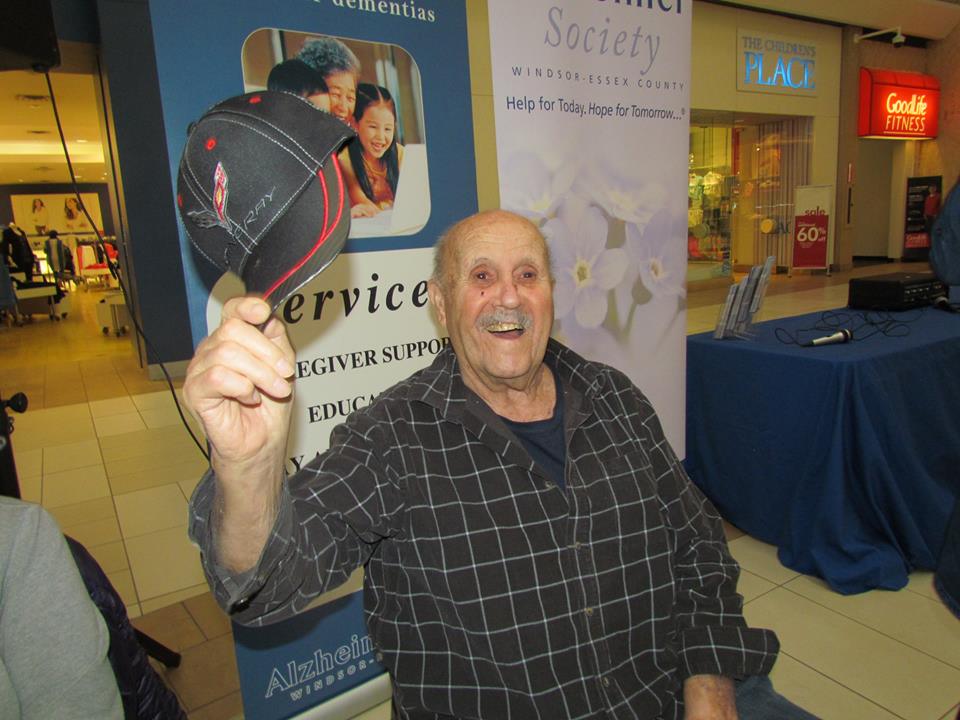
It has been just over two weeks since Ernie moved into Mississauga’s Erin Mills lodge, and his daughter Marlene has seen a noticeable improvement. The move, she says, is “bringing new life back to Dad.”
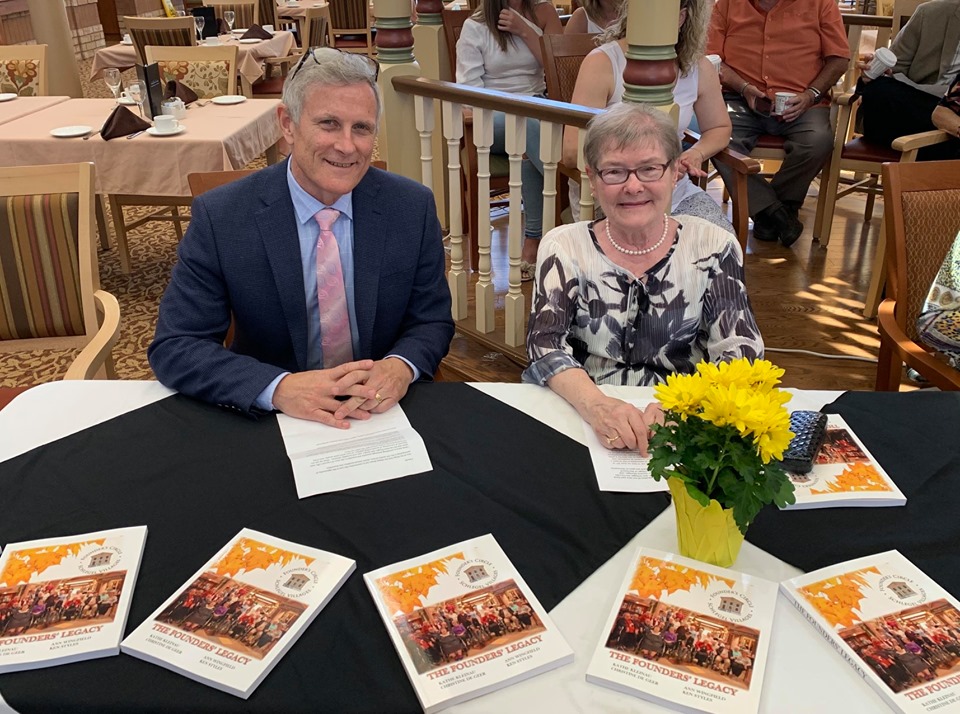
“They have been so absolutely lovely,” says one family
member about the team at Erin Mills Lodge and the care
the small home offers her father and his fellow residents.
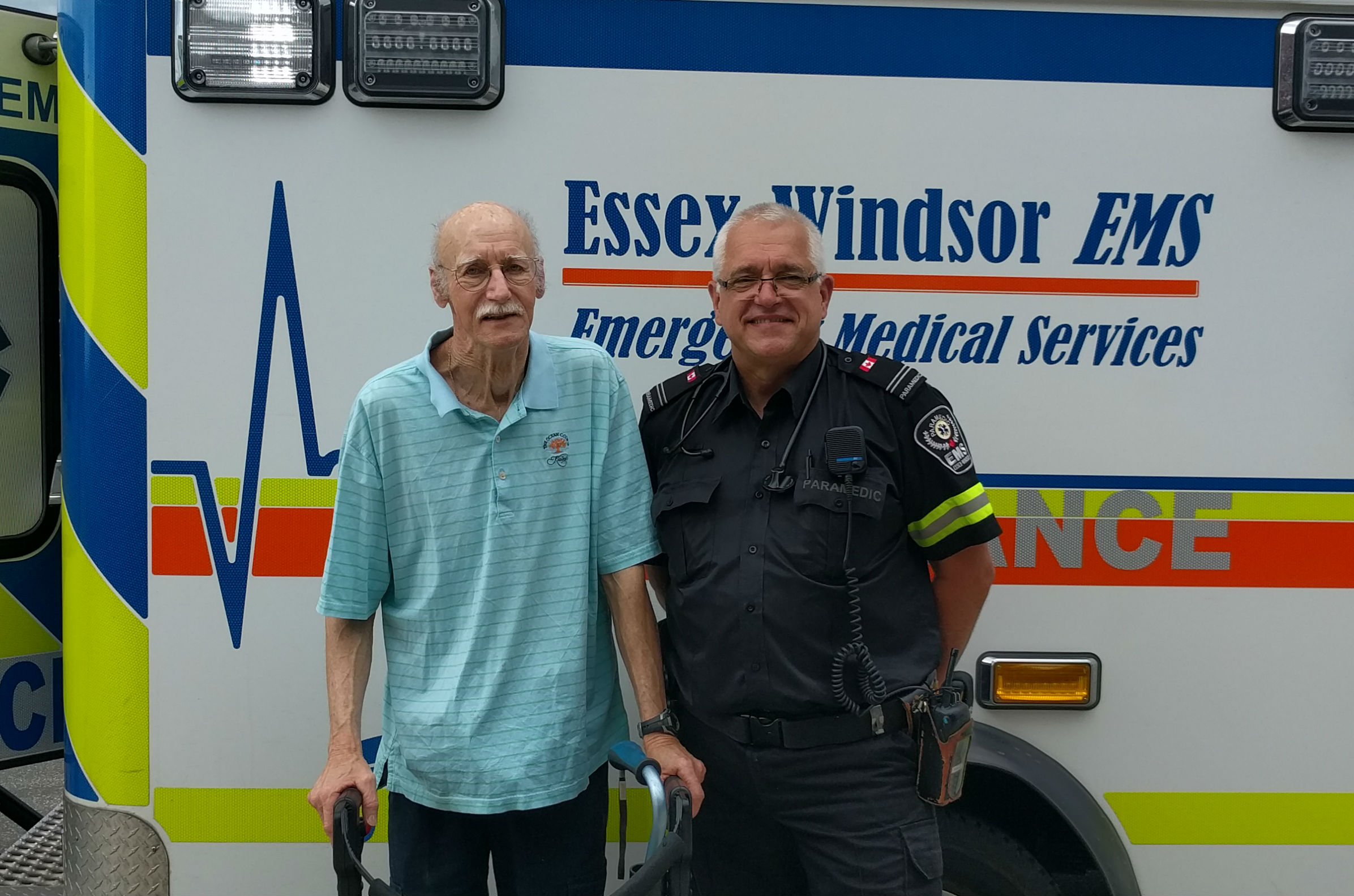
Ernie has been living with the progression of dementia for some time and in the fall of 2020, it was agreed it was time for Ernie to transition from living with family into a long-term care home with more supports available. His needs began to rapidly change in early 2021, however, and he began to experience more anxiety on a regular basis. His ability to communicate verbally further diminished and it was difficult to understand him and to communicate with him. As his expressions escalated, it got to the point where Ernie had to be hospitalized.
While at the hospital, he continued to struggle. The staff at the hospital were caring and patient, Marlene says, and they regularly provided the family with updates from the various health professionals involved in her father’s care. They continued to try and find the correct medication regimen to help alleviate some of Ernie’s anxiety as well as other aspects of his dementia, but there seemed to be little change. It became clear his long-term care home would not be able to provide the kind of care Ernie now required.
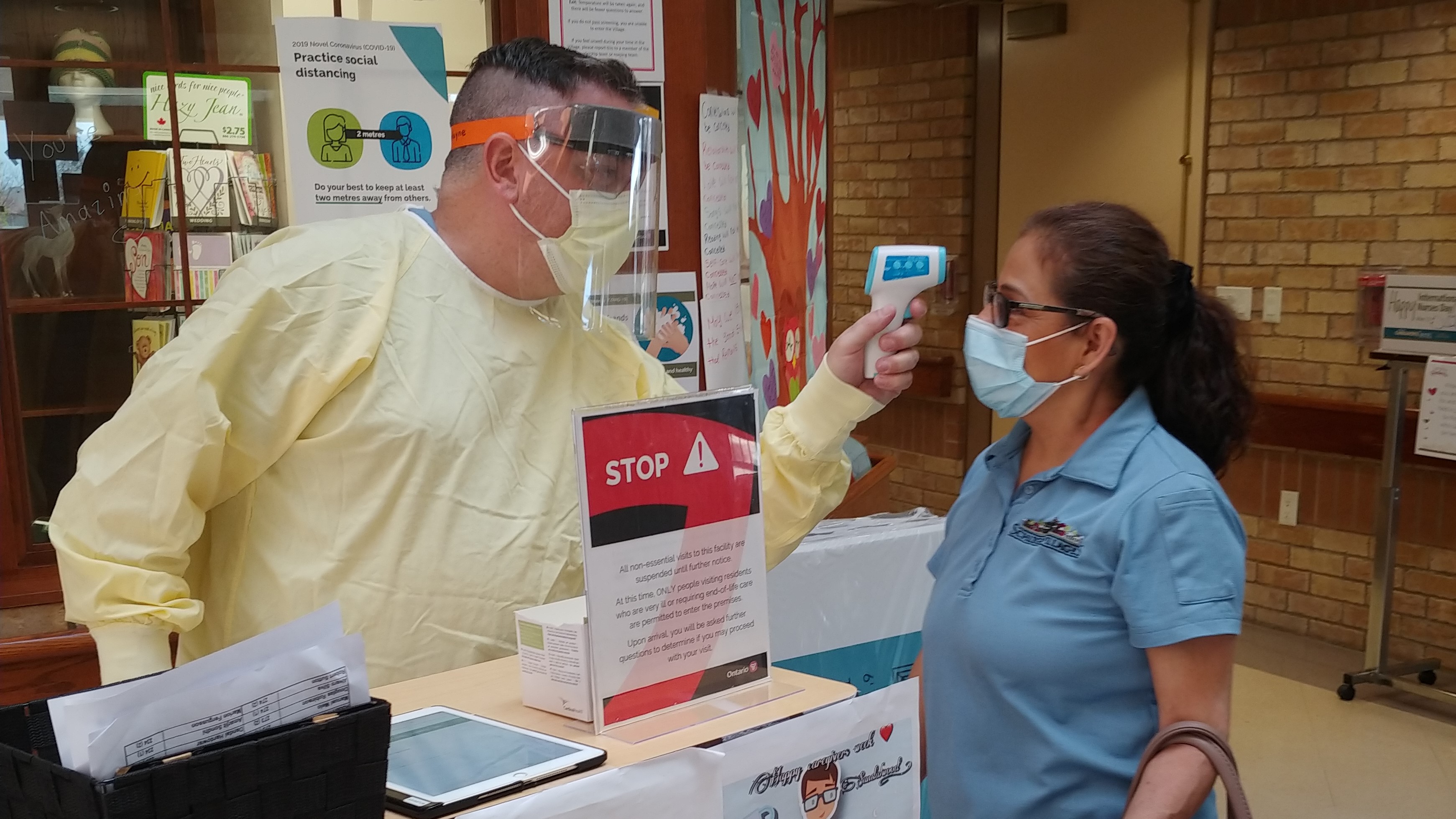
All of this was at a time when COVID-19’s third wave threatened to overwhelm Ontario’s hospital system and the leaders of the acute care sector reached out to their partners in Long-Term Care to seek any and all assistance. In order to create desperately-needed space, hospitals needed to find long-term care homes willing and able to welcome Alternate Level of Care (ALC) patients like Ernie, and they needed it done quickly.
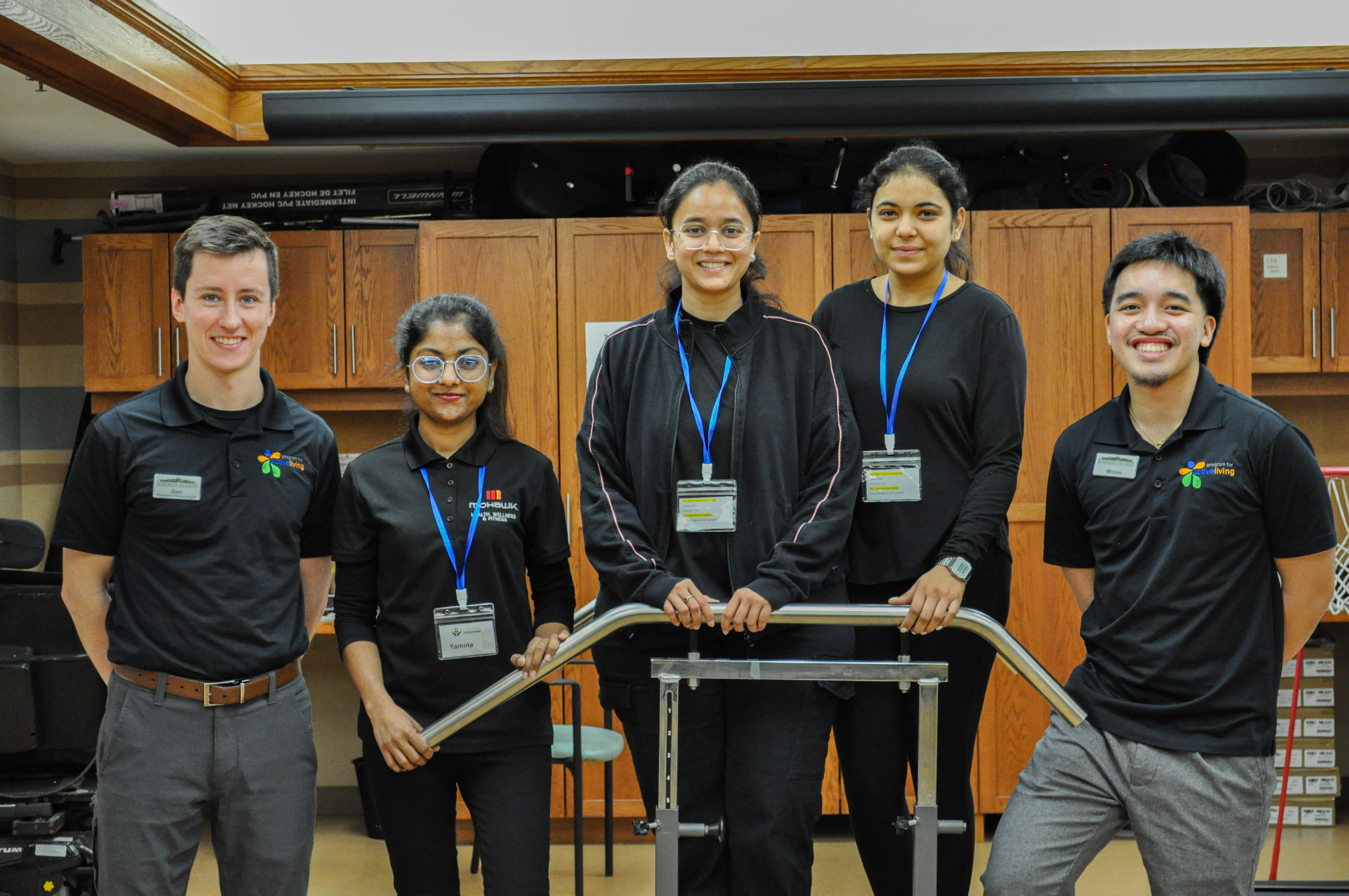
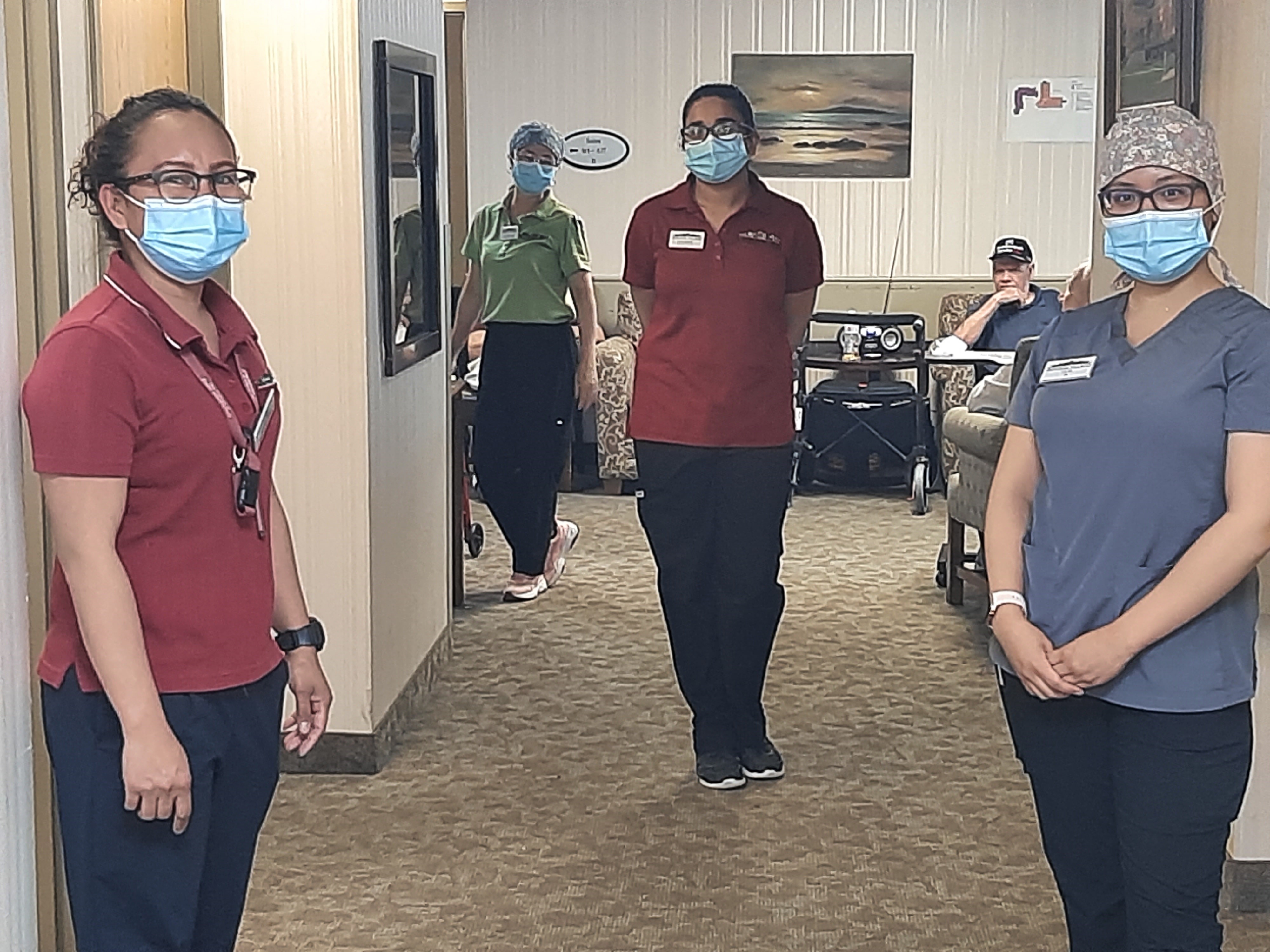
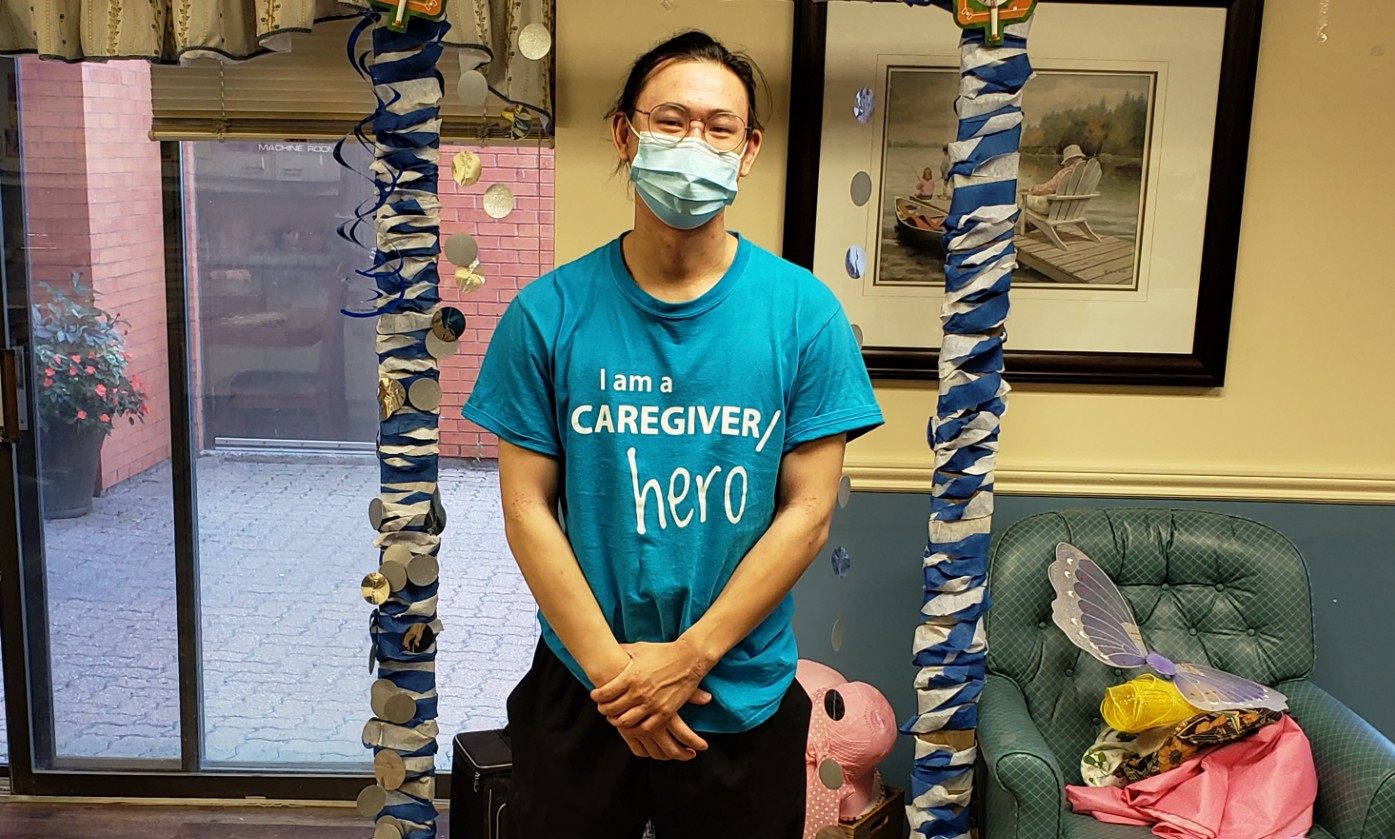
Ernie’s case was considered to be complex. There were both physical and emotional challenges together with the regular cognitive challenges brought about by dementia. Few long-term care homes were equipped to provide the type of care Ernie now required. Erin Mills Lodge, however, didn’t hesitate and quickly offered to pilot a new initiative for such residents. The small home had one empty floor set aside for cohorting should a COVID-19 outbreak occur, which meant they could accept 20 people with complex needs safely in one neighbourhood. Perhaps more importantly, the team at Erin Mills Lodge has a deeply-ingrained understanding of the individual nature of dementia and other complex diagnoses, so they knew they could meet Ernie’s needs.
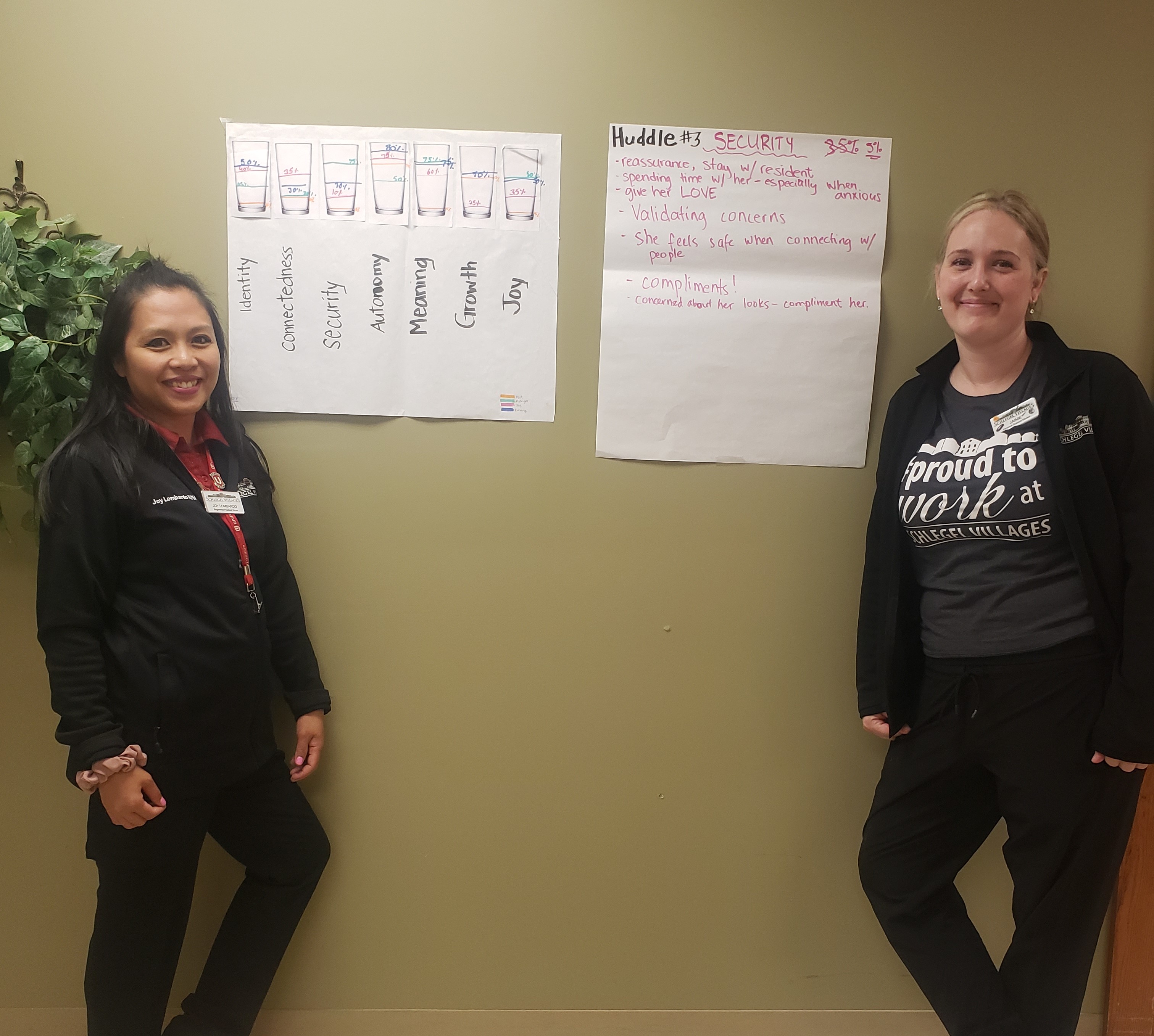
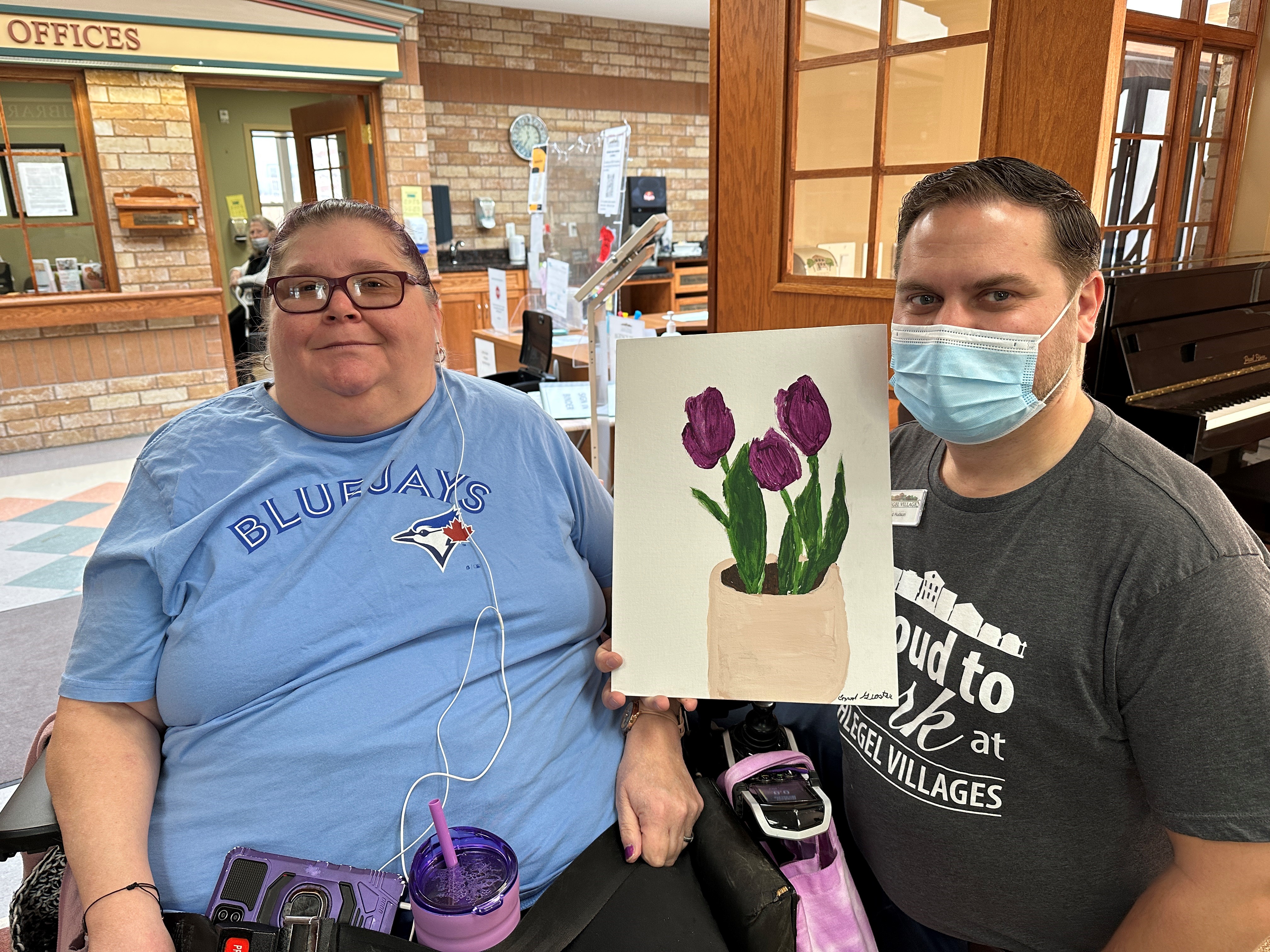
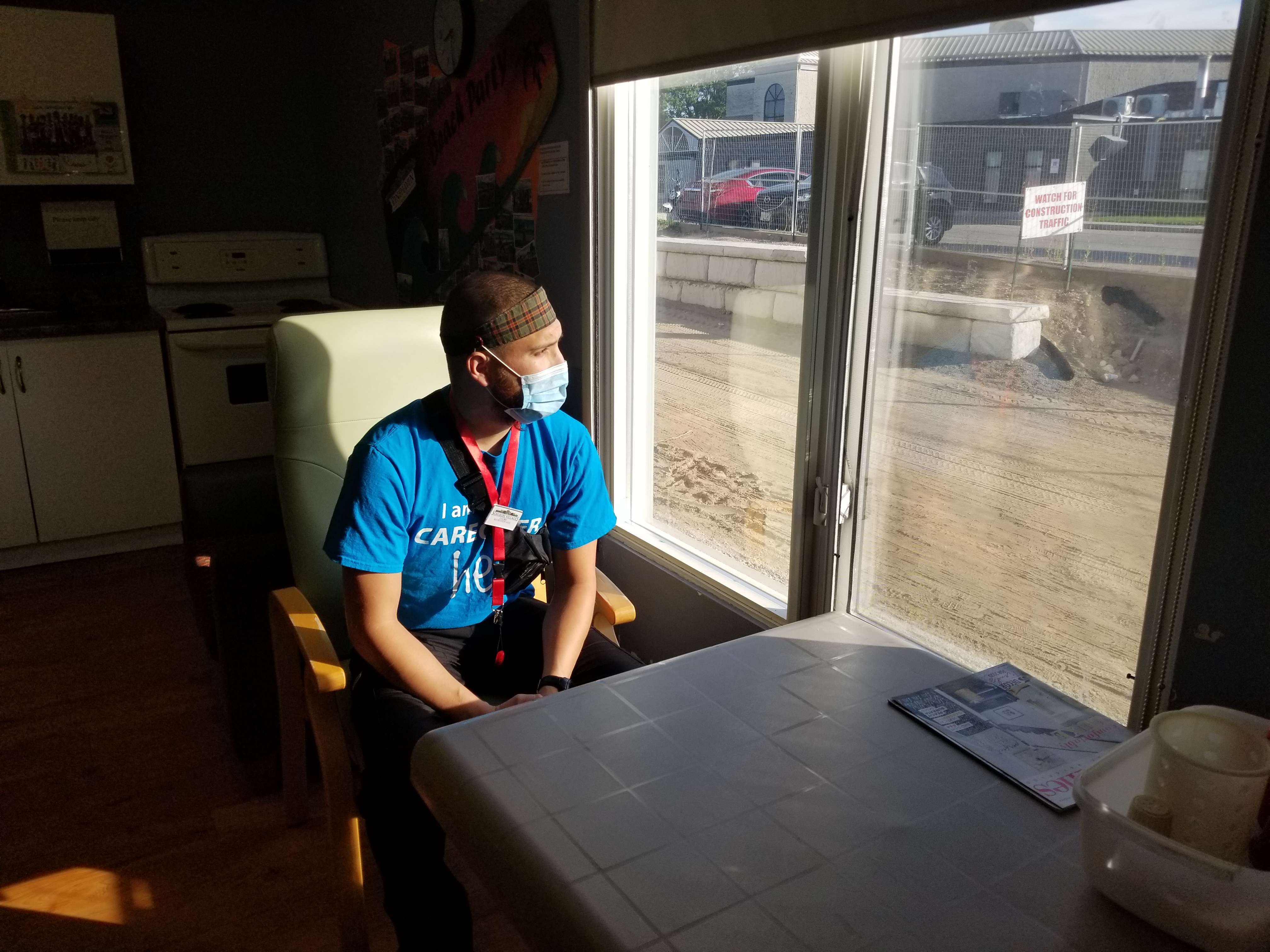
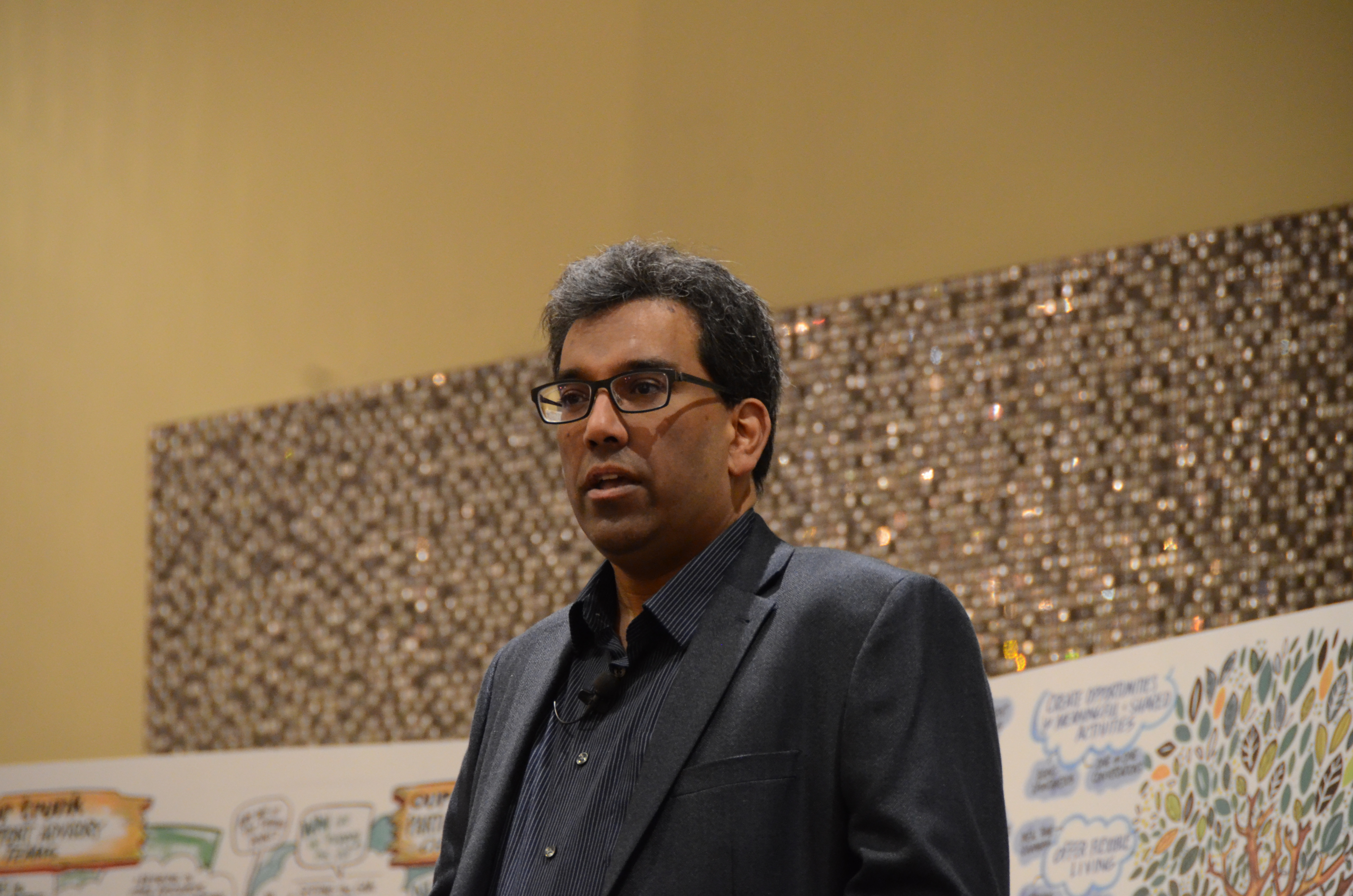
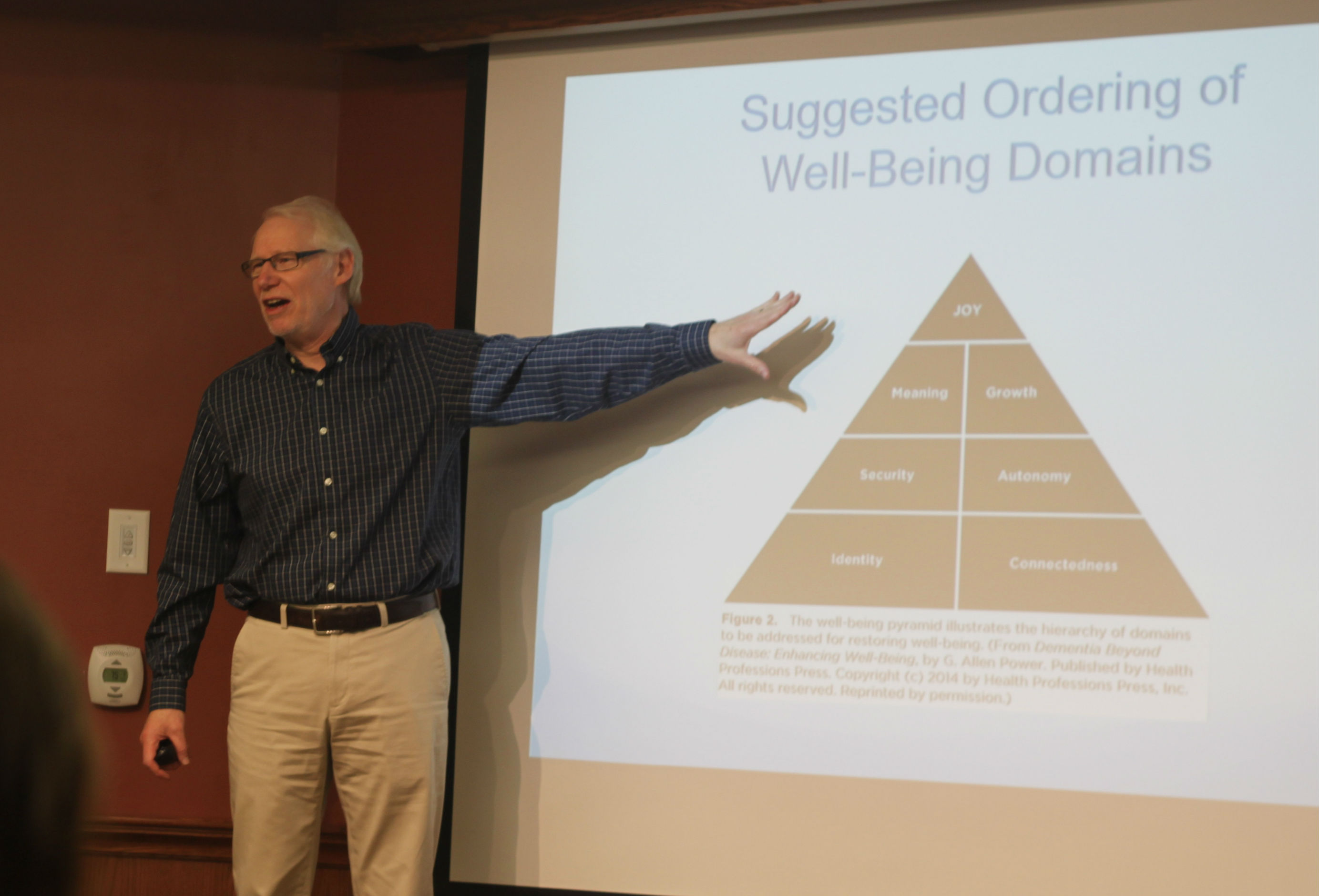
Erin Mills Lodge General Manager Sutha Vinayaga says that no matter the care needs a person may have, a combination of environment and engagement can be the basis for more comfort hour-to-hour and day-to-day. He says the “patient files” the team have received for everyone who has moved in contained a lot of “behavioural” red flags, yet when they were welcomed and made comfortable by the team, Sutha didn’t see any of them emerge.”
“It is the environment and the way they were welcomed in that helped them quickly adapt, like they had come home,” Sutha says.
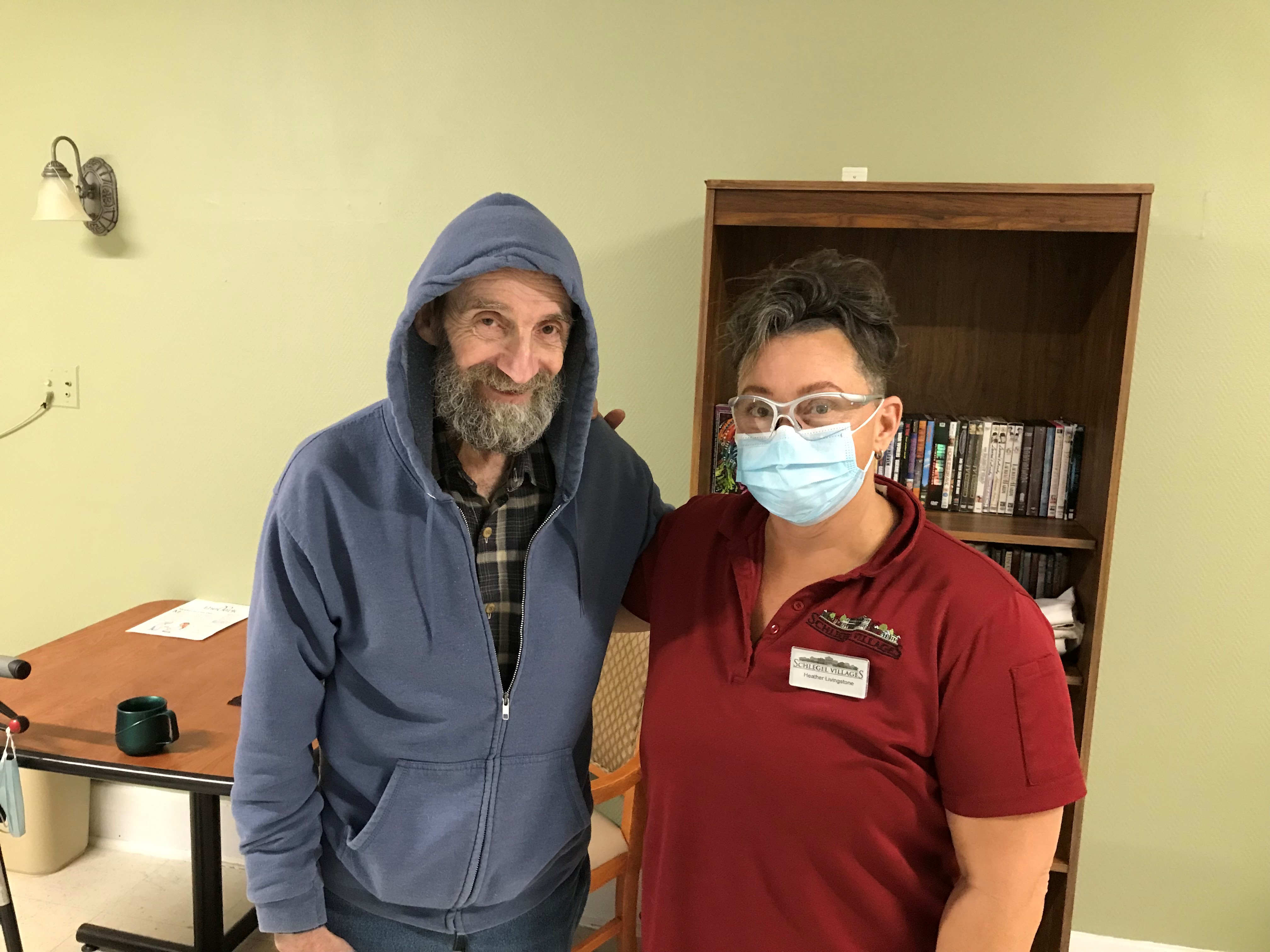
“It’s moving from the clinical to a beautiful, caring home setting that is still very safe and secure,” Marlene says. “I don’t think it would be as successful a program, however, without the people at the home. It’s about trying to meet Dad where he is; the word that keeps coming to mind is ‘grace’. People have just had such grace in dealing with Dad’s various challenges. I have seen him find more peace and be more settled since coming to EML.”
“They have been so absolutely lovely,” she says.
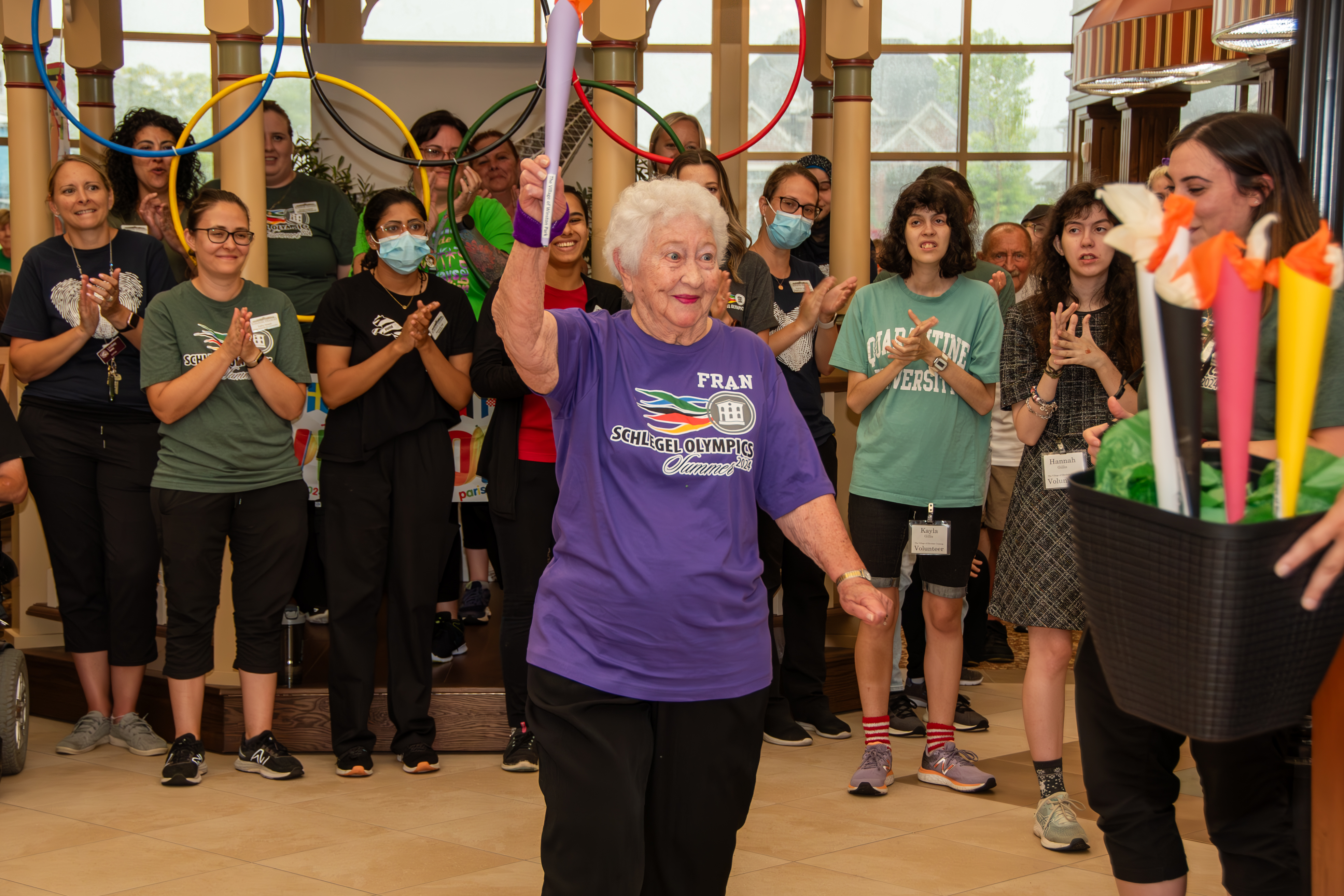
As of June 17, 20 people who were struggling for peace in hospital settings have come to Erin Mills Lodge, and the team is proud to see how well people are adjusting. With patience, they take time to get to know each person so they might understand how best to meet them in the moment, taking each interaction as a thought to nothing more than the present.
In doing so, a small measure of harmony is found for the new residents and the families who love them.
Note: This pilot program is designed to provide 20 temporary LTC beds specifically designated for referrals from hospitals in communities around Erin Mills Lodge. This Enhanced Supportive Neighbourhood (ESN) has specific additional resources beyond the regular LTC program capabilities to enable solutions for residents experiencing difficulty finding a home to meet their long-term needs. The ESN seeks to assess, stabilize and find care-planning strategies on a temporary basis of approximately 60-180 days. During this transitional period, residents and their families are supported in finding acceptance to a permanent LTC home that meets their preferences and needs. The program has shown evidence of meeting these needs in a safe and licensed residential setting that not only considers a person’s clinical health requirements but also nurtures their social and emotional well-being in a manner hospitals were never designed to achieve.